Newly Created Cells Better at Repairing Myelin in Preclinical Study
Therapeutics designed to produce new oligodendrocytes — the cells responsible for the protective myelin sheath that is damaged in multiple sclerosis (MS) — might be the most effective approach for disorders such as MS, according to a study conducted in a fish model.
That’s because oligodendrocytes that survive being damaged in MS produce far less myelin than newly created cells. They also send the myelin to the wrong part of the nerve much more often, researchers say.
In contrast, newly generated oligodendrocytes give rise to abundant and correctly placed myelin sheaths.
“Improving our understanding of what happens after myelin becomes damaged is one of our research priorities, and studies like this take us another step closer to our important goal of stopping MS,” Clare Walton, PhD, head of research at the MS Society U.K., said in a press release.
“We’re really proud to have helped fund this latest study from Edinburgh, which could have important implications for future MS treatment,” she added. “MS is relentless, painful and disabling, and we need to find ways to repair damaged myelin so no one has to worry about their MS getting worse.”
The study, “New oligodendrocytes exhibit more abundant and accurate myelin regeneration than those that survive demyelination,” was published in the journal Nature Neuroscience in the form of a brief communication.
MS is caused by an erroneous immune attack against the protective myelin sheath on nerve fibers, which is required for efficient nerve cell communication and to protect nerve cells from degeneration.
Restoring lost myelin (remyelination) after damage is vital to preserve and potentially restore nerve function. Thus, after damage occurs, new oligodendrocytes are generated from progenitor cells to form new layers of myelin and put them on the correct place in nerve cells.
Recent research suggests that some oligodendrocytes that survive the immune attacks can also go on to produce new myelin, but to what extent these cells contribute to myelin regeneration remains unknown.
To address this question, researchers at the MS Society Edinburgh Centre for MS Research used a zebrafish model to compare remyelination abilities of surviving oligodendrocytes to those of newly generated cells.
The fish were first exposed to a chemical called capsaicin to induce demyelination, or the loss of myelin. This led to a 95% reduction in myelinated nerve fibers, but there were only 33% fewer oligodendrocytes in these animals, “indicating that many oligodendrocytes survived demyelination,” the team wrote.
There was also an increased number of new oligodendrocytes, which allowed the “investigation of remyelination by both surviving and newly generated oligodendrocytes,” the researchers added.
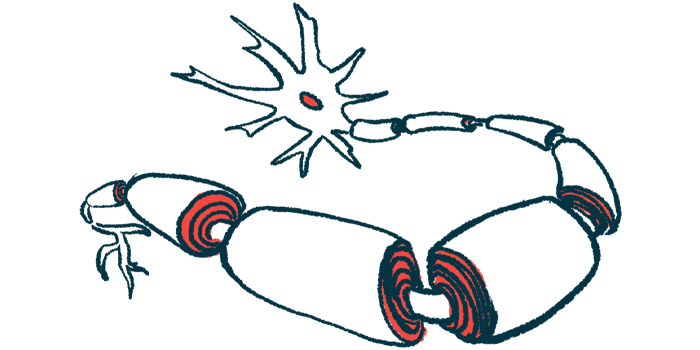
The fate of individual surviving oligodendrocytes was followed before and after capsaicin-induced demyelination. Imaging analysis showed that surviving oligodendrocytes generated myelin sheaths of normal length but made very few of them — two per cell on average, compared to 18 before demyelination.
In addition, about half of the surviving oligodendrocytes misdirected newly made myelin to the bodies of nerve cells. Normally, myelin surrounds nerve fibers only, which extend from the nerve cell body.
The team then attempted to promote remyelination by blocking an enzyme called ROCK which, under control conditions, would increase the number of myelin sheaths produced by oligodendrocytes. After demyelination, however, blocking ROCK did not affect the number of sheaths made by surviving oligodendrocytes. Instead, it increased myelin misplacement.
“Collectively, our data indicate that surviving oligodendrocytes have a limited capacity to form new myelin sheaths in vivo [within the living organism],” the scientists wrote.
To confirm that the mistargeting of myelin is also seen in MS, postmortem brain samples from five MS patients, donated to the MS Society U.K. Tissue Bank, were compared to samples from five people who did not have MS.
The number of nerve cell bodies that were abnormally surrounded by myelin was nearly 100 times higher in patients’ brain samples than in normal samples, indicating that “myelin mistargeting is a previously unappreciated feature of MS,” the scientists noted.
The team finally examined newly generated oligodendrocytes to determine whether mistargeted myelin was a general feature of all oligodendrocytes or specific to surviving cells.
Results showed that new oligodendrocytes produced 25 sheaths per cell on average — 10-fold more than surviving oligodendrocytes — and that nearly all newly created sheaths were correctly placed on nerve fibers, “demonstrating that myelin mistargeting is a feature of remyelination by surviving oligodendrocytes,” the investigators wrote.
“Our analyses reveal limited and aberrant remyelination by oligodendrocytes that survive demyelination and suggest that therapeutic strategies to promote remyelination through the generation of new oligodendrocytes might be the most promising approach for demyelinating disorders, such as MS,” they concluded.