FAQs about Kesimpta
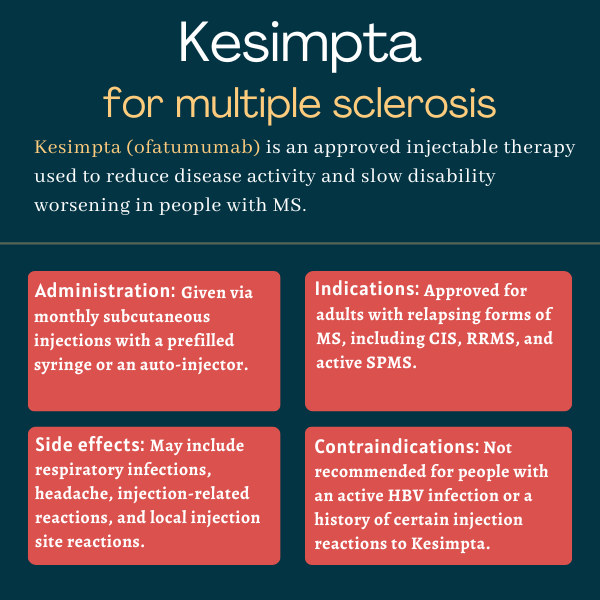
Kesimpta was approved by the U.S. Food and Drug Administration in August 2020 to treat adults with relapsing forms of multiple sclerosis (MS). It can be prescribed for patients with clinically isolated syndrome, relapsing-remitting MS, and active secondary progressive MS. Ofatumumab was initially approved in 2009, under the brand name Arzerra, for patients with chronic lymphocytic leukemia.
Kesimpta may cause fetal harm. The medication is not recommended for use during pregnancy. Those who can become pregnant are advised to use birth control during treatment and for six months after stopping the therapy.
No known interactions exist between Kesimpta and alcohol. However, given that alcohol can interfere with some medications and disease symptoms, patients are advised to discuss with their healthcare teams whether it is safe for them to drink.
Kesimpta results in rapid B-cell depletion that can be observed as early as after one week of treatment, but it may take several months for its clinical effects to become evident. Because each person may react to a treatment in a different way, patients are advised to discuss with their healthcare providers how Kesimpta may help them.
Hair loss and weight gain have not been reported in studies as side effects associated with Kesimpta. Patients are advised to talk with their healthcare team if they experience any such issues.
Related Articles

 Fact-checked by
Fact-checked by