Plasmapheresis for MS
Plasmapheresis is a procedure that’s sometimes used to manage severe multiple sclerosis (MS) relapses when corticosteroids are not effective or cannot be tolerated. The therapy works by filtering harmful substances out of the blood that are thought to drive relapse symptoms.
MS is caused by the immune system mistakenly attacking healthy parts of the brain and spinal cord, known as the central nervous system, leading to inflammation and nerve damage. In relapsing forms of MS, people experience periods of new or worsening symptoms, known as relapses or flare-ups, followed by periods of recovery (remission) where symptoms ease or disappear.
The first-line approach for managing severe flares is glucocorticoids, a class of corticosteroid medications with powerful anti-inflammatory and immunosuppressive properties. When these steroid medications cannot sufficiently control a severe flare or are not well tolerated, plasmapheresis may be considered as a second-line therapy.
What is plasmapheresis?
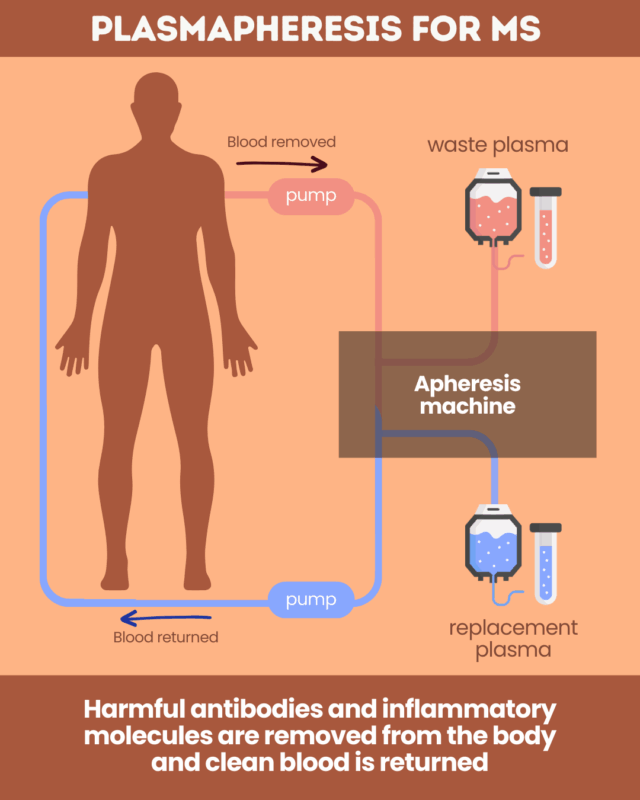
Blood contains several types of cells, including red blood cells, white blood cells, and platelets, all suspended in a liquid called plasma. Plasma is where the harmful antibodies and inflammatory molecules believed to drive MS relapses are found. Removing these proteins can help speed recovery from a relapse and ease symptoms.
Plasmapheresis, also called therapeutic plasma exchange, is a filtering procedure designed to remove these problematic substances from the blood and help control a severe MS relapse.
During the procedure, blood is removed from the body and passed through a specialized machine that separates the plasma from the blood cells. The plasma is discarded and replaced with a substitute fluid or fresh frozen plasma from a healthy donor. The “cleaned” blood is then returned to the body through the other arm.
Who may benefit from plasmapheresis
For severe relapse treatment, plasmapheresis is mainly used in people with relapsing-remitting MS (RRMS) who have failed to improve with high-dose steroids.
Studies suggest that about 40%-60% of RRMS patients who do not respond to steroids may experience at least moderate functional improvement after the procedure. Still, the effect of plasma exchange in these MS patients can vary. Better outcomes are generally observed in younger patients, those with shorter disease durations, and individuals who initiate treatment within two weeks of relapse onset.
Plasmapheresis is not usually recommended for people with progressive forms of MS, including primary progressive MS and secondary progressive MS. Some patients can still experience relapses, but the role of plasma exchange in these forms of MS remains understudied.
The procedure may also be used in rare instances where a person develops a serious infection, such as progressive multifocal leukoencephalopathy, while taking certain antibody-based disease-modifying therapies. In these rare cases, plasmapheresis is used to remove the medication from the bloodstream more quickly to restore the immune system’s ability to fight the infection.
Beyond MS, plasmapheresis is also used for other conditions in which harmful blood components contribute to symptoms, including myasthenia gravis and thrombotic thrombocytopenic purpura.
Risks and side effects of plasmapheresis
As with any treatment, plasmapheresis for MS can come with certain risks and side effects. The most common include:
- low blood pressure, which may cause weakness, dizziness, nausea, or fainting
- feeling cold or experiencing chills
- mild tingling or cramping caused by low calcium levels
- minor allergic reactions, such as rash or fever, to the plasma replacement fluid
- fatigue
Less common, but potentially serious complications may include:
- severe allergic reactions to the plasma replacement solution
- electrolyte imbalances
- increased susceptibility to bleeding
- blood clots
- infections
The plasmapheresis procedure: What patients can expect
Plasmapheresis can be performed as either an inpatient or outpatient treatment, but it is always conducted by a healthcare provider.
For MS, treatment typically involves three to seven sessions in total, scheduled daily or several times per week. Each session generally lasts two to four hours.
While the exact regimen can vary, the procedure will usually involve:
- Vein access: Needles are placed into the veins, usually one in each arm, to draw blood out and return it after filtration. An anticoagulant may be administered to prevent the blood from clotting during the procedure.
- Plasma separation: Blood from one arm flows into a specialized device called an apheresis machine, which separates the blood cells from the plasma. The plasma, which contains the harmful antibodies and inflammatory molecules, is discarded.
- Plasma replacement and reinfusion: A replacement fluid is combined with the remaining blood cells inside the machine, and this mixture is returned to the body through the needle in the other arm.
This cycle of blood removal and reinfusion is automated and continuous, so only a small amount of blood is outside the body at any given time.
Patients will be monitored throughout the process for changes in blood pressure or other side effects. After a session, people are usually advised to rest and drink plenty of fluids for the next 24 hours.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

