Stressful Environment Triggers Inflammatory Cells Linked to Autoimmune Diseases Like MS, Study Shows
Written by |
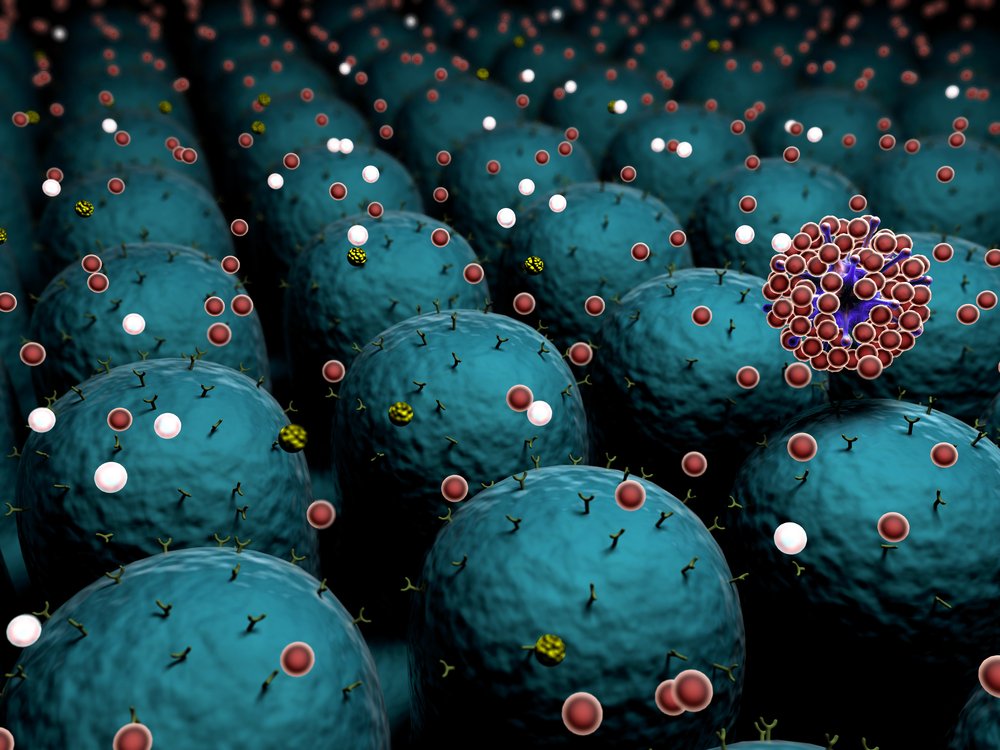
A stressful microenvironment, characterized by low metabolites and low oxygen levels, triggers the generation of immune cells directly implicated in a variety of inflammatory diseases, such as multiple sclerosis (MS).
The study, “Cellular Stress in the Context of an Inflammatory Environment Supports TGF-β-Independent T Helper-17 Differentiation,” was published in the journal Cell Reports.
Immune cells are vital players defending our organism not only against pathogens but also by doing surveillance and cleanup of harmful cells, such as cancer cells. T-cells, a type of white blood cell, are part of our immune system army and their function is tightly regulated by factors present in their microenvironment.
T-cells can be recast into different cell subtypes, such as Th17 cells, so that tailored immune responses are set in motion. The activation and differentiation of these cells when unregulated, however, can contribute to the development of autoimmune diseases, including MS.
How alterations in the local environment influences the transformation of T-cells into Th17 cells has been poorly understood.
Now, a team of researchers at the Instituto de Medicina Molecular (iMM) in Lisbon, Portugal, tackled this question and showed that a stressful environment, characterized by low levels of oxygen and shortage of metabolites, such as glucose, enhances the generation of Th17 cells.
Researchers used both stress inducers and pharmacological stress inhibitors and observed that while stress inducers enhanced the development of Th17 cells, inhibiting stress reduced their development.
Using an MS mouse model — the experimental autoimmune encephalomyelitis (EAE) model — researchers observed that administering mice with stress inhibitors significantly delays the onset of signs of EAE when compared to control mice.
Overall, the results suggest that “adverse metabolic environments during inflammation provide a link between adaptive immunity and inflammation and may represent a risk factor for the development of chronic inflammatory conditions by facilitating Th17 cell differentiation,” the team concluded in their study.
Marc Veldhoen, the study’s lead author and group leader at iMM, said to Multiple Sclerosis News Today, “Our study shows that those white blood cells actively involved in autoimmune disorders such as MS and arthritis, Th17 cells, are preferentially generated in situations where cells experience stress. This stress can be due to reduced availability of energy, such as in the form of low oxygen or sugar levels.”
“Targeting cellular stress pathways may provide an opportunity to reduce the generation of cells contributing to disease, thereby alleviating disease symptoms and patient suffering. In addition, it could provide insights into the circumstances in which disease may recur, the largely unknown environmental triggers, thereby reducing disease relapses,” Veldhoen concluded.