Swedish Study Suggests Stem Cell Transplants as Possible Treatment for Aggressive RRMS
Written by |
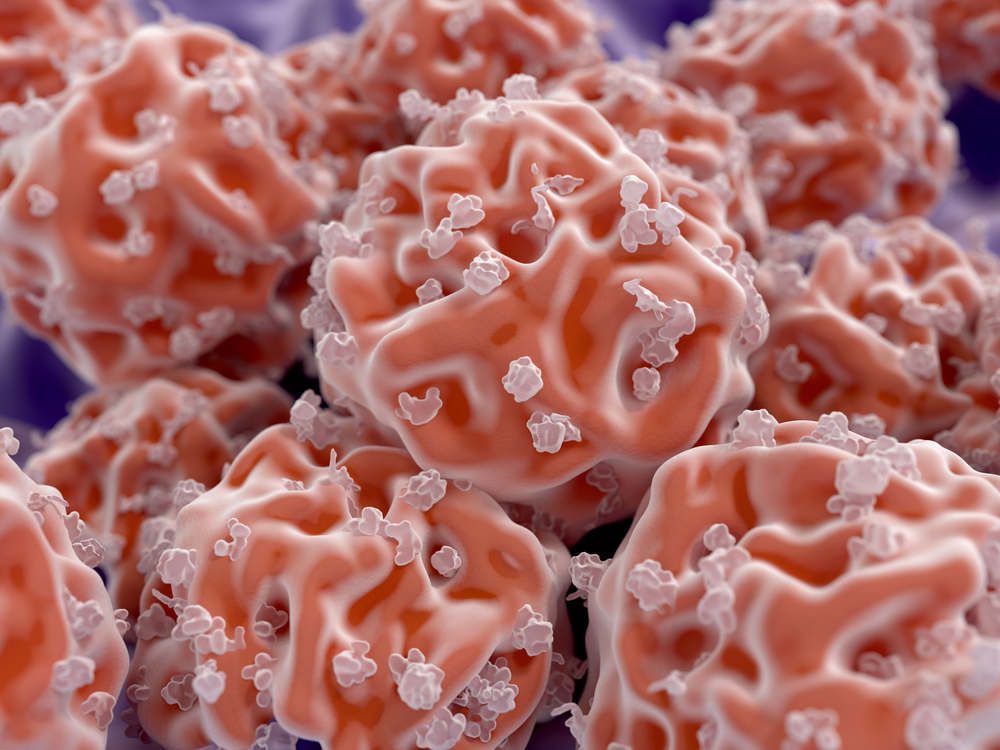
Autologous hematopoietic stem cell transplants for relapsing-remitting multiple sclerosis (RRMS) are superior to currently approved disease-modifying drugs, according to a Swedish study published in the Journal of Neurology, Neurosurgery & Psychiatry.
In addition, says the review, the procedure’s safety profile has improved in the last decade, and is now just as good as approved medications.
This data supports the idea that bone marrow stem cell transplants could be recommended for RRMS patients who don’t respond to treatment with disease-modifying drugs if the procedure is performed at experienced centers, argued researchers at Sweden’s Uppsala University.
Yet they said the benefits of stem cell transplants for patients with progressive disease is moderate at best — meaning any attempts to treat these patients with a stem cell transplant should be limited to clinical trials.
A mishmash of studies
In reviewing data of stem cell procedures in MS, the report, “Autologous haematopoietic stem cell transplantation for neurological diseases,” noted that available studies vary considerably in the type of patients recruited, as well as procedures used for the transplant. They all have serious limitations, it said.
Many such studies are based on patient registries, yet they suffer the serious flaw of unvalidated data. In a clinical trial, data is always verified in numerous ways, but in a registry study, information on, for instance, disease stage is not double-checked.
Physicians scoring patients are not certified — as is the case in clinical trials — and have varying levels of experience. Moreover, since patients are not selected according to inclusion criteria, participants vary widely in their characteristics.
They are also treated according to varying protocols and in centers with varying experience levels. In fact, studies have shown that inexperienced treatment centers increase the risk of death after stem cell transplants in MS. In addition, many uncontrolled studies contribute with data.
The team identified four studies that included at least 10 RRMS patients. In total, the studies analyzed had 188 RRMS patients, but again, treatment protocols and data reporting varied among the studies. All this makes interpreting their findings difficult, researchers said, as it is often impossible to directly compare study outcomes.
So far, one published randomized controlled clinical trial of stem cell transplants in MS exists: the Autologous Haematopoietic Stem Cell Transplantation trial in MS (ASTIMS) study (EUDRACT No. 2007-000064-24).
Indications of efficiency
Despite the variability among the uncontrolled studies, researchers concluded that clinical and imaging outcomes are rather consistent between studies.
The ASTIMS clinical trial reported that new inflammatory lesions, assessed by magnetic resonance imaging (MRI), fell by 79 percent, and by 64 percent in annualized relapse rates compared to mitoxantrone — an immunosuppressive treatment used in highly active disease states. But the results were reported as a combined measure for RRMS and secondary progressive MS (SPMS) patients, of which only seven had relapsing disease.
Two of the uncontrolled studies reported no MRI activity of any sort in 85 percent and 86 percent of participants at five years. A study that had used a harsh conditioning regimen reported that none of the patients had imaging signs of the disease up to 10 years after the treatment.
Studies also reported a halted progression of disability of 70 to 91 percent at five years. Researchers observed that the lowest numbers were found in groups with a higher proportion of patients with SPMS.
No evidence of disease activity (NEDA) has lately emerged as a robust outcome measure in studies of MS therapies. This comprehensive measure takes into account disease activity in MRI scans, the presence of relapses and disability progression.
A number of studies showed that 68 to 70 percent of patients maintained NEDA four to five years after a transplant. In comparison, in a group of patients treated at Boston’s Brigham and Women’s Hospital, only 7.9 percent had NEDA at seven years, even though most of them had been treated with disease-modifying drugs.
Meanwhile, in clinical trials of newer drugs such as Tysabri (natalizumab) or Lemtrada (alemtuzumab), only 32 to 39 percent of patients maintained NEDA at two years.
Finally, researchers noted that clinical trials or other studies of Tysabri or Tecfidera (dimethyl fumarate) found no improvements in patients’ health-related quality of life. In contrast, one study of transplanted MS patients showed an improvement of nearly four times what is considered as a clinically meaningful improvement at two years. Improvements were seen in both physical and mental health.
A second study that used a different analysis tool reported a 15-point increase among transplanted patients. Researchers consider eight points to be clinically relevant.
Safety
Although it’s becoming increasingly clear that stem cell transplants offer profound benefits for RRMS patients, the procedure’s safety concerns limit its endorsement.
For a stem cell transplant to have an impact, doctors must first get rid of a patient’s faulty immune system. They do this with the help of a so-called conditioning regimen. These can be of high, medium or low intensity, and the safety issues of a transplant are usually related to acute or long-term toxic effects of this pretreatment, rather than the transplanted cells.
The amount of acute toxicity is directly linked to the intensity of the conditioning regimen. High-intensity regimens use chemotherapy or radiation to completely wipe out the immune system, while milder protocols stick to immunosuppressive treatments.
Acute toxic effects include hair loss, reduction of blood cell counts and the presence of bacteria in the bloodstream — side effects that are often manageable. Far less is known about long-term side effects, though. These can come in the form of viral reactivations including shingles, development of other autoimmune conditions, impaired fertility and a higher potential risk of cancer — all of which make for a serious knowledge gap, researchers said.
In fact, acute effects have been linked with deaths among MS patients undergoing stem cell transplants. But researchers showed that while early studies showed unacceptably high death rates — 5.3 percent in a 2006 report and 3.8 percent in a 2010 report — studies of newly transplanted patients show far better outcomes.
One study that looked only at patients transplanted after 2005 found a treatment-related mortality rate of 0.3 percent, which is on par with that reported in clinical trials of Lemtrada. The same study found no deaths among patients who had a mild-intensity pretreatment.
The improved numbers might be related to the wider use of mild-intensity conditioning regimens, but also to more experience among treatment centers, researchers said.


