Inactivation of S1PR2 Protein Shows Therapeutic Potential in MS Mouse Model, Study Reports
Inactivation of S1PR2, a cell surface protein, helps improve clinical disability and reduce demyelination in a mouse model of experimental autoimmune encephalitis (EAE), a condition similar to multiple sclerosis (MS) in humans, a study shows.
This finding suggests that therapies blocking S1PR2 could have the potential to treat MS.
The study, “Inactivation of sphingosine-1-phosphate receptor 2 (S1PR2) decreases demyelination and enhances remyelination in animal models of multiple sclerosis,” was published in the journal Neurobiology of Disease.
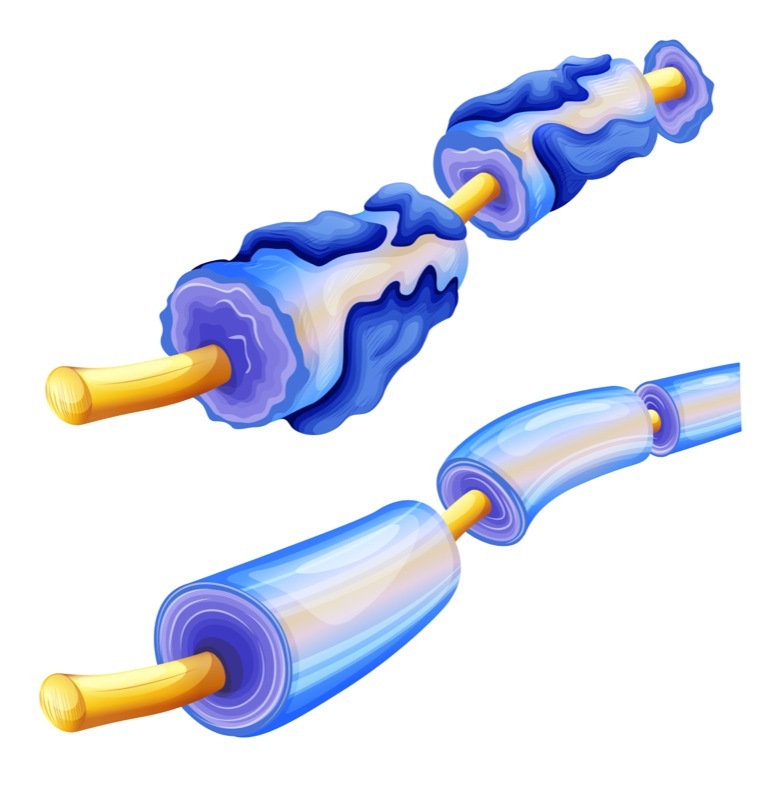
MS is an inflammatory disease of the central nervous system that develops as a result of damage to the protective cover of nerve cells, known as the myelin sheath, in the brain and spinal cord in a process called demyelination.
Patients with MS often develop multiple sites of breakdown in the blood-brain barrier — a highly selective barrier that separates the circulating blood from the brain. This barrier breakdown leads to the entrance of unwanted substances into the brain, including high levels of immune cells. Once inside the brain, these immune cells cause damage to the myelin sheaths.
Sphingosine-1-phosphate receptor 2 (S1PR2) is a cell surface receptor — a protein that resides on a cell surface that, when activated, carries out certain signaling pathways. A previous study had shown that inactivation of S1PR2 reduced blood-brain barrier leakage, and improved behavioral deficits in a rodent EAE model.
However, the role of S1PR2 in myelin repair has not yet been investigated.
Therefore, researchers set out to determine whether S1PR2 inactivation would lead to a decrease in demyelination by regulating properties of the blood-brain barrier.
Through the use of a toxin called lysolecithin, the researchers created an experimental model of demyelination in the adult mouse spinal cord. Next, they investigated the role of S1PR2 by inactivating the protein using either the pharmacological inhibitor JTE-013, or by deleting the S1PR2 gene using a process called gene knockout.
As hypothesized, the researchers discovered that inactivation of S1PR2 led to improved myelin repair mechanisms, and higher numbers of remyelinated neurons at the sites of damage. Furthermore, S1PR2 inactivation was associated with an increased production of oligodendrocytes — the cells that produce myelin.
MS patients frequently experience disturbed visual function due to demyelination of optic nerves — nerves that transmit signals to the brain from the retina at the back of the eye. Interestingly, S1PR2 inactivation in mice led to improved behavioral outcomes in an optokinetic reflex test, which tests eye movement in response to objects moving in the periphery while the head is stationary.
Next, the researchers studied the effects of S1PR2 inactivation on blood-brain barrier permeability, demyelination, and remyelination processes in an EAE mouse model.
Results indicated that S1PR2 inhibition using JTE-013 or gene knockout improved blood-brain barrier permeability, decreased the extent of demyelinated areas, and improved clinical disability in this EAE model.
Based on the results, the team concluded “S1PR2 activity impairs remyelination and also enhances BBB [blood-brain barrier] leakage and demyelination.”
Blocking S1PR2 showed a dual benefit “in demyelinating, MS-like lesions: better protection of the BBB against damage and smaller lesions on one hand, and enhanced oligodendrocyte differentiation and remyelination on the other hand,” the researchers added.
The team suggests that therapies selectively blocking S1PR2 could be potential therapeutic agents against MS.






