Excess of Single Transcription Factor Appears to Hinder Myelin Repair by Oligodendrocytes, Study Finds
Written by |
Unusually high levels of a transcription factor called paired related homeobox protein 1 (PRRX1) in human oligodendrocyte progenitor cells hinders their ability to respond to the loss of myelin and to transform into mature, myelin-producing oligodendrocytes, a new study shows.
These findings suggest a new potential way of treating multiple sclerosis (MS), one targeting therapies that can prevent or overcome this block in the maturity of these precursor cells by moving them out of a state called pathological quiescence (inactivity).
The study, “Paired Related Homeobox Protein 1 Regulates Quiescence in Human Oligodendrocyte Progenitors,” was published in the journal Cell Reports.
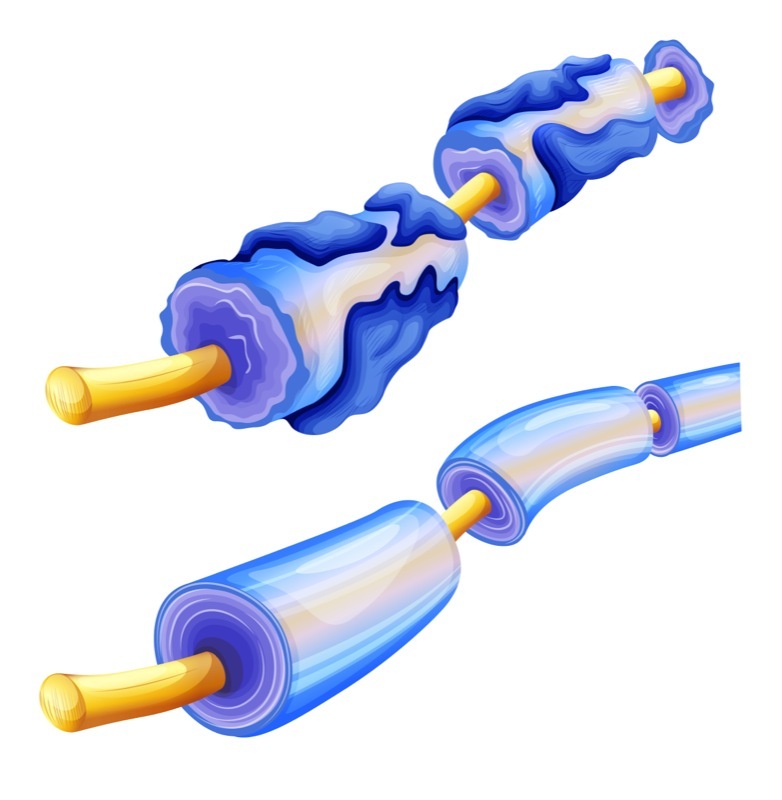
Oligodendrocytes, the myelin-producing cells, develop from more immature, stem cell-like cells called oligodendrocyte progenitor cells. These are the cells that, upon myelin loss, travel to demyelinated lesion sites where they mature and generate myelin-producing cells.
In vivo loss of a single oligodendrocyte progenitor cell, through death or because they transformed (differentiated) into a mature oligodendrocyte, is a tightly regulated process, but its mechanisms remain poorly defined.
These progenitor cells, much like other stem cell-like cells in adult tissues, exist in a state of dormancy called cellular quiescence. This dormancy is essential for maintaining cell populations in reserve for when a tissue needs regeneration and repair.
In muscle stem cells, loss of quiescence leads to the exhaustion of the stem cell pool and failed regeneration. However, failure to “wake” the cells from this dormant state after an injury — what researchers call pathological quiescence — may also contribute to failed regeneration.
Researchers at the University at Buffalo (UB) had previously identified several transcription factors whose levels were higher in human oligodendrocyte progenitor cells than was seen in progenitor cells that give rise to neurons.
Want to learn more about the latest research in MS? Ask your questions in our research forum.
In this study, they investigated the function of one of these transcription factors — PRRX1 — in the regulation of human oligodendrocyte progenitor cells.
Results showed that increased levels (overexpression) of PRRX1 suppressed the proliferation of human oligodendrocyte progenitor cells, leading to an arrest in cell division and promoting a state of stem cell quiescence.
“We found that switching this gene on could cause problems in myelin repair by blocking the proliferation of the oligodendrocyte progenitor cell, the stem cell-like precursor that is responsible for all myelin regeneration in the adult brain,” Fraser Sim, PhD, an associate professor of pharmacology and toxicology in the Jacobs School of Medicine and Biomedical Sciences at UB and the study’s lead author, said in a UB news release written by Ellen Goldbaum.
Moreover, high PRRX1 (specifically one of its two variants, called PRRX1a) levels impaired a cell’s ability to migrate, an essential feature in MS since these progenitor cells are required to travel to the sites of myelin loss (the loss of myelin is a hallmark of MS).
Researchers then assessed the impact of PRRX1 overexpression in a mouse model of leukodystrophy, a group of rare, genetic diseases characterized by an abnormal development or destruction of the myelin sheath in the central nervous system (brain and spinal cord).
Results showed that PRRX1a overexpression significantly hindered the human oligodendrocyte progenitor cell’s ability to colonize the brain’s white matter, and to induce effective myelin regeneration or remyelination.
Researchers confirmed that overexpression of PRRX1 induced a gene expression signature associated with quiescence. They also found that two pro-inflammatory signaling molecules, called interferon-gamma and bone morphogenetic proteins (BMP), increased the expression of PRRX1 and promoted quiescence.
Blocking the expression of PRRX1 prevented the damage caused by these pro-inflammatory molecules.
“We found that blockade of PRRX1 expression prevents the negative effects of interferon-γ, suggesting that PRRX1 expression might be a viable target in inflammatory diseases, such as multiple sclerosis, where interferon-γ may prevent successful myelin regeneration,” said Sim.
Developing therapies capable of inducing human oligodendrocyte progenitor cells to mature into myelin-producing oligodendrocytes is an approach of interest in the MS field. These new findings suggest one option may lie in blocking the induction of pathological quiescence in these cells.
“The idea that pathological quiescence of progenitors could prevent regeneration in MS is distinct from the current pre-clinical strategies making their way into trial,” Sim said.
“We plan to pursue the idea that perhaps we could identify treatments for MS that work by overcoming pathological quiescence of oligodendrocyte precursors in demyelinating lesions that characterize this disease,” he concluded.


