Study of Myelin Debris Sheds Light on Brain Inflammation in MS
Endothelial cells, those lining the inside of small blood vessels, promote clearance of myelin debris — a common detrimental outcome of demyelinating diseases such as multiple sclerosis (MS) or spinal cord injury. However, in its path to clear the brain from myelin debris, endothelial cells trigger more damaging mechanisms, promoting inflammation, and the formation of abnormal blood vessels and scar tissue.
The study with that finding, “Microvascular endothelial cells engulf myelin debris and promote macrophage recruitment and fibrosis after neural injury,” was published in the journal Nature Neuroscience.
Myelin, the fat-rich substance that wraps around nerve fibers (axons), works to insulate and increase the velocity of the signals relayed by nerve cells of the central nervous system (brain and spinal cord).
In MS, as well as in patients with spinal cord injury where axons are destroyed, the breakdown of myelin causes myelin debris to accumulate in the injured areas, impairing axon regeneration and remyelination, and contributing to further inflammation. This ongoing inflammation contributes to MS progression, and triggers secondary injury cascades in the case of patients with spinal cord injury.
Uncontrolled inflammation “persists for a long period of time following a spinal cord injury. We know that myelin debris acts as an inflammatory stimulus that exacerbates secondary injury by activating other cells in the injured spinal cord that are actively involved in inflammatory responses during disease progression,” Yi Ren, the study’s co-lead author, said in a press release. Ren is professor of biomedical sciences at the Florida State University College of Medicine.
As a result, efficiently removing myelin debris is key for recovering the injured tissue.
“Clearing myelin debris generated at the time of injury is critical in controlling the inflammatory response and to ensuring neural regeneration,” said Ren.
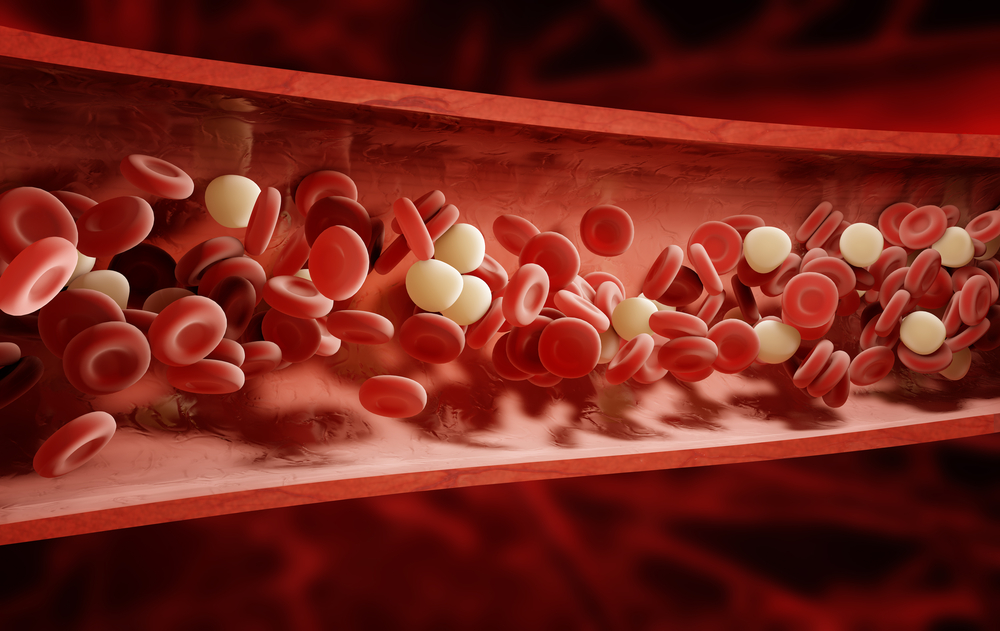
Macrophages, a specialized white blood cell and the big “eaters” of our immune system, are the main players in clearing myelin debris. Another player is microglial cells, the central nervous system’s immune cells. However, macrophages and microglia cells are usually absent from the injury site, suggesting the existence of another player.
This new player, researchers found, are endothelial cells, those that line the interior of small blood vessels and act as “amateur eaters” to engulf myelin debris.
Using mouse models of spinal cord injury and MS (the experimental autoimmune encephalomyelitis model, EAE), researchers found that upon damage, the endothelial cells are activated to remove myelin debris and other potentially damaging material from the sites of injury.
However, while endothelial cells uptake myelin and activate the signalling pathways for its clearance, they trigger a series of mechanisms associated with disease progression.
“The consequences of the effort of endothelial cells to clear myelin debris is often severe, contributing to post-traumatic degeneration of the spinal cord and to the functional disabilities often associated with spinal cord injuries,” Ren said.
Endothelial cell’s clearance of myelin triggers an abnormal formation of new blood vessels (a process called angiogenesis) at the injury site, as well as chronic inflammation; once activated, endothelial cells recruit large amounts of macrophages to the injured site, promoting inflammation. Finally, the uptake of myelin particles and its elimination process performed by endothelial cells contributes to the development of “scar tissue” also known as fibrosis.
“Unexpectedly, we found that the process of engulfing debris confers upon endothelial cells the ability to stimulate production of fibrotic components suggesting that these cells have a function in the formation of fibrotic scars. Specifically, they facilitate the arrival of macrophages derived from bone marrow that ultimately promote chronic inflammation,” Ren said.
Overall, the findings shed light on a so far unknown mechanism promoting inflammation, scar tissue, and abnormal blood vessel formation in demyelinating disorders, like MS and spinal cord injury.
According to the team, therapeutics that target the mechanisms now identified may help halt and even reverse the damaging effects of myelin uptake by endothelial cells.






