Tiny Cell Membrane Disruptions Lead to Nerve Fiber Degeneration in MS, Mouse Study Suggests
Written by |
Tiny ruptures in the cell membrane of nerve fibers enable the entry of calcium and ultimately lead to their degeneration, a study in a mouse model of multiple sclerosis (MS) suggests.
The study, “Calcium Influx through Plasma-Membrane Nanoruptures Drives Axon Degeneration in a Model of Multiple Sclerosis,” was published in the journal Neuron.
The extent of the degeneration of nerve fibers, or axons, that occurs in MS patients correlates with the degree of their disability. Prior work from a team at Ludwig-Maximilians-Universität München (LMUM) demonstrated that nerve fiber degeneration is initially characterized by swelling and cellular changes, such as damage in the mitochondria (which provide energy to cells) and impaired transport of molecules. While some nerve fibers then experience fragmentation, others recover.
“In some cases, the swelling spontaneously regressed and these axons recovered. So the process is in principle reversible, and could perhaps be therapeutically modulated if we had a better understanding of the underlying mechanisms,” Martin Kerschensteiner, MD, the study’s senior author and the director of the Institute of Clinical Neuroimmunology at LMUM, said in a press release.
Interestingly, calcium concentration within the nerve fiber could determine which ones will recover, as suggested by studies linking increased calcium levels to axon degeneration and neuroinflammatory lesions.
Aiming to explore this association further, the team from LMUM and the Technical University of Munich induced experimental autoimmune encephalomyelitis (EAE) in mice — similar to MS in humans — with a calcium sensor in their neurons.
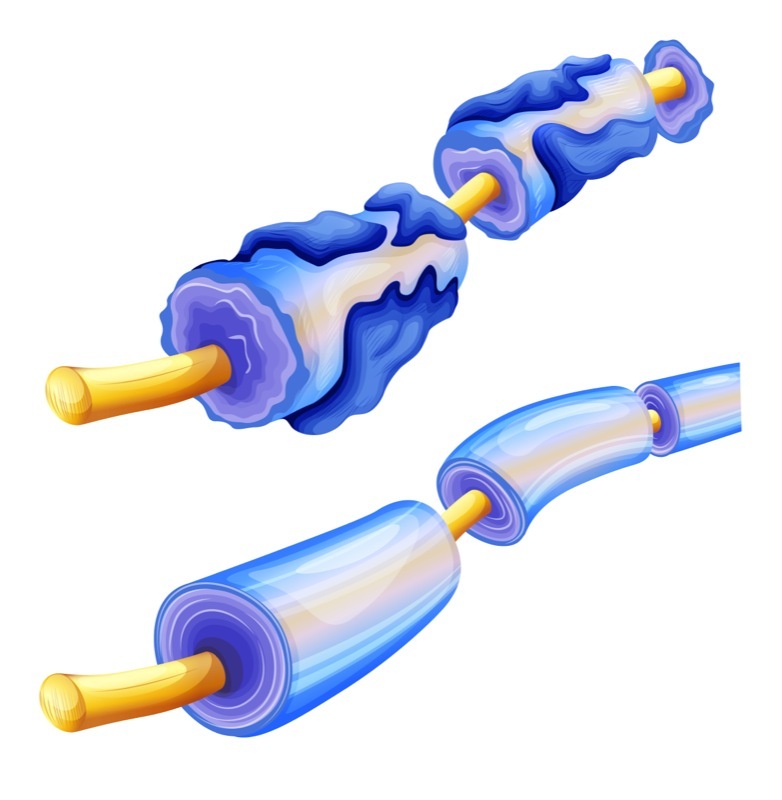
By measuring calcium levels in nerve fibers using spinal in vivo imaging, the investigators found that calcium accumulates early during degeneration. In 10% of the nerve fibers, calcium was already increased before the onset of swelling. Approximately half of the swollen axons had high levels of calcium and an associated high risk of degeneration.
When the team monitored these fibers over several hours, they observed that this calcium accumulation predicted axonal fate. Within an hour, about 4% of normal-appearing axons showed a calcium rise, of which a substantial proportion (16% per hour) progressed to swelling. In contrast, nerve fiber swelling without prior calcium increase was seldom observed. Nerve fibers able to clear calcium were able to recover, while those maintaining abnormally high levels likely swelled and degenerated.
Then, the team identified the extracellular space — where calcium concentration is about 10,000-fold higher than in the cell — as the major source of the degeneration-associated excess calcium. Scientists observed this after they removed calcium from the extracellular space, which normalized calcium levels in nerve fibers and induced their recovery.
Subsequent experiments in control and EAE animals using a fluorescent dye showed that calcium entered spinal nerve fibers via nanoscale disruptions in the cell membrane, as had been shown in studies of traumatic central nervous system injuries. The observations also suggested that these tiny ruptures — likely the result of toxic mediators, according to the researchers — are already present at the early stages of fiber damage, and correlate with local inflammation.
“The complex [with the fluorescent dye] is too large to penetrate into an intact axon. Only if the membrane has been damaged can it be taken up into the axon,” Kerschensteiner said.
Dye uptake appeared to be more pronounced in fibers showing loss of their protective layer, called myelin. Furthermore, the researchers “were also able to show that many of the axons that take up the dye also contain increased amounts of calcium,” he added.
“We thus propose calcium permeable membrane nanoruptures as a novel mechanism of inflammatory axon injury,” the scientists wrote in the study.
The finding that nerve fibers with disrupted membranes are able to recover implies that stabilizing membranes against such attacks and the machinery of cell membrane repair are potential treatment targets, the researchers said.
“The fact that, in the inflamed nervous system, tears in the cell membrane can contribute to the death of nerve fibers is a new discovery, which could in future be therapeutically relevant,” said Thomas Misgeld, MD, a study co-author and a professor at the Institute for Neuronal Cell Biology at TUM.


