FAQs about Extavia
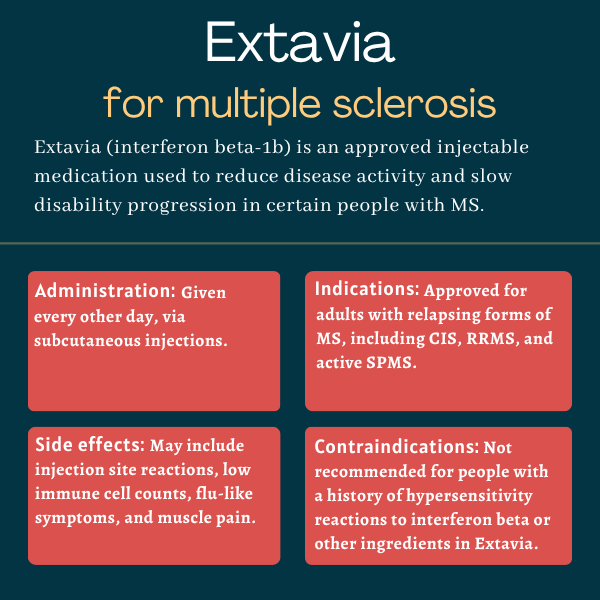
Extavia was approved by the U.S. Food and Drug Administration in August 2009 to treat adults with relapsing forms of multiple sclerosis (MS), including clinically isolated syndrome, relapsing-remitting MS, and active secondary progressive MS.
However, the active ingredient in Extavia, interferon beta-1b, was originally approved in 1993 under the brand name Betaseron.
Although there are no well-controlled studies examining the effects of Extavia exposure during pregnancy, observational studies have not found an increased risk of major birth defects or other adverse pregnancy outcomes. If clinically necessary, Extavia may be used during pregnancy, but a discussion with a healthcare provider is strongly recommended for anyone planning to become pregnant while on Extavia.
There is no known interaction between Extavia and alcohol. However, Extavia may cause liver damage, which is also a known complication from alcohol use. Patients should talk with their healthcare team about whether it is safe for them to drink alcohol while on Extavia.
Multiple sclerosis is a disease that manifests differently in each person, so it’s difficult to predict when Extavia will start to have an effect. Patients should ask their care team how and when the medication is expected to help in their case.
Both hair loss and weight gain have been reported as potential side effects of interferon beta-1b, the active ingredient in Extavia. Patients who experience these or other side effects during treatment are advised to discuss them with their healthcare team.
 Fact-checked by
Fact-checked by