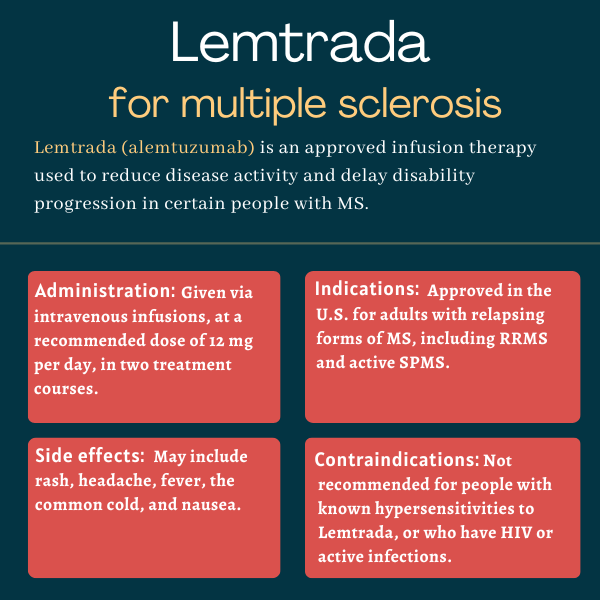
FAQs about Lemtrada
Lemtrada was approved by the U.S. Food and Drug Administration in November 2014 for the treatment of adults with relapsing forms of multiple sclerosis (MS), including relapsing-remitting MS and active secondary progressive MS. Its active ingredient, alemtuzumab, had originally been approved in 2007 for blood cancer, under the brand name Campath.
Lemtrada has not been well studied during pregnancy in humans, but research in animals suggests it may cause harm to a developing fetus. Patients who are able to become pregnant should use contraception while on Lemtrada, and for four months after each treatment course.
There are no known interactions between Lemtrada and alcohol. However, drinking alcohol can potentially exacerbate some multiple sclerosis symptoms or side effects associated with the medication. Safe alcohol use should be discussed with a person’s healthcare team, who can make the best recommendation based on each particular case.
In clinical trials, Lemtrada induced a rapid and marked depletion of immune B-cells and T-cells within a few days of infusion. However, it is unclear when the medication starts to impact clinical measures of disease or specific symptoms. Patients are advised to discuss with their healthcare providers how Lemtrada can help them.
While hair loss was not reported in clinical trials as a side effect of Lemtrada, some patients who received the medication in real-world settings have noted this issue. The treatment also can cause thyroid problems, which may result in unexplained weight gain or weight loss. Patients who experience any unexpected side effects are advised to talk with their healthcare team.
 Fact-checked by
Fact-checked by