Multiple sclerosis diagnosis: Testing for MS
Diagnosing multiple sclerosis (MS) can be challenging because there is no single test that can confirm or rule out the neurodegenerative disease. However, an early MS diagnosis is crucial, as it enables earlier treatment, which typically results in better clinical outcomes.
MS is characterized by inflammatory damage in the brain and spinal cord, collectively known as the central nervous system (CNS), resulting from an immune system malfunction.
Diagnosing MS often involves a range of different imaging and laboratory tests to determine whether the characteristic patterns of inflammation and nervous system damage are present.
Who diagnoses multiple sclerosis?
Depending on a person’s symptoms, several doctors may be involved in diagnosing MS, including primary care physicians, ophthalmologists, or emergency physicians. Specialists are better equipped to diagnose MS, interpret specialized tests, and determine the appropriate next steps after a diagnosis is established.
Ultimately, a definitive MS diagnosis is typically made by a neurologist, a medical doctor who specializes in the diagnosis, treatment, and management of disorders affecting the nervous system.
What criteria do doctors use to diagnose MS?
Because there is no single MS diagnosis test, the process usually involves:
- a detailed medical history, including current and past symptoms, and a person’s family history
- a neurological exam for MS that assesses for problems with balance, coordination, and other potential MS symptoms
- imaging and laboratory tests that help confirm MS and rule out other conditions
The McDonald Criteria for MS diagnosis, most recently revised in 2024, are a set of diagnostic parameters that provide standardized guidelines to facilitate the correct identification of MS.
According to these criteria, four main types of evidence can be assessed that could suggest damage characteristic of MS:
- dissemination in space, or signs of damage in at least two different areas of the CNS
- dissemination in time, or signs of damage that have occurred at different points in time
- characteristic MRI features, or specific patterns of tissue damage on MRI scans
- laboratory evidence of CNS inflammation, such as the presence of specific markers in the cerebrospinal fluid (CSF), the liquid surrounding the CNS
Another essential aspect of these MS diagnosis criteria is ruling out other conditions that can cause similar neurological symptoms.
What tests are used to diagnose MS?
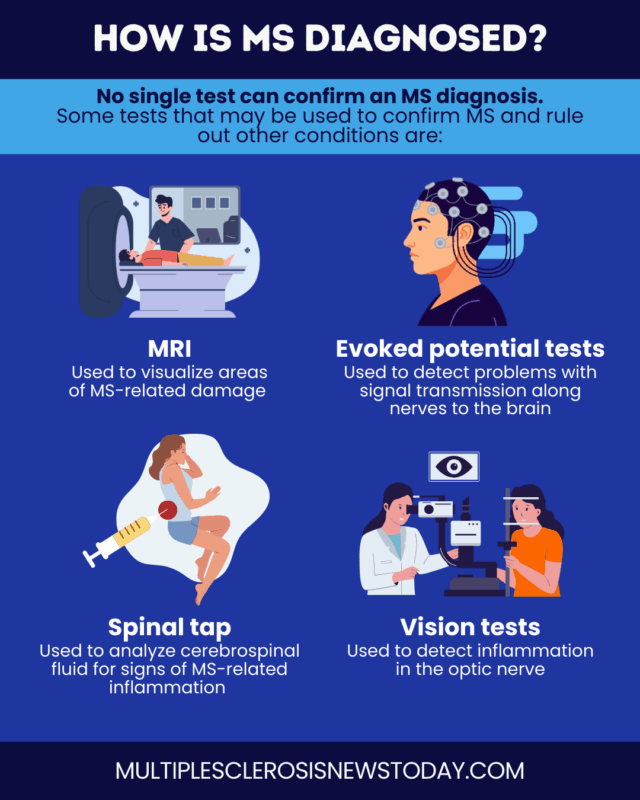
Several diagnostic tests may be used to help confirm an MS diagnosis.
Magnetic resonance imaging
Known simply as MRI, magnetic resonance imaging is the preferred imaging tool for diagnosing and tracking the progression of MS. The noninvasive technique uses strong magnetic fields and radio waves to produce detailed images of tissues without exposing a patient to radiation.
MRI can reveal MS lesions — areas of inflammation and damage to the myelin sheath, a fatty substance that surrounds nerve cells — that are characteristic of the disease. MS lesions on MRI may appear brighter or darker than healthy tissue, depending on the type of scan used.
While various types of MRI scans exist, diagnosing MS with MRI typically involves:
- T2-weighted scans, which show the total number of lesions, both old and new. Some of the most common include:
- MRI scans
- evoked potential tests
- spinal tap
- vision tests
- T1-weighted scans with contrast, which can detect lesions with active inflammation
Evoked potential tests
Evoked potential tests are used to measure the speed at which electrical signals travel along sensory nerves to the brain. Damage caused by MS can slow these signals, sometimes even before symptoms are noticeable.
These tests typically involve placing small electrodes on the scalp to record the brain’s electrical response to visual, auditory, or sensory stimuli.

Living with MS
Mental health and MS
Living with MS
Symptoms of MS vision problems

Living with MS
High-dose vitamin D delays MS progression
The most commonly used test for diagnosing MS is called visual evoked potential, which assesses the brain’s response to a visual pattern displayed on a screen. This test checks for issues with signal transmission along the optic nerve, the nerve that carries signals between the eyes and the brain, which is a common site of MS-related damage.
Spinal tap
A spinal tap, also known as a lumbar puncture, involves collecting a small sample of CSF via a small needle inserted between the vertebrae in the lower back.
In MS, CSF analysis may reveal oligoclonal bands, which are antibodies indicating CNS inflammation, as well as kappa free light chains, which are faster and easier to measure but provide similar information to oligoclonal bands. These findings can support an MS diagnosis when combined with clinical and MRI evidence.
A spinal tap for MS may also be used to measure levels of immune cells or other proteins associated with inflammation or nerve damage.
Vision tests
About 20% of people with MS will experience optic neuritis, or inflammation of the optic nerve, as their first symptom. Vision tests for MS are often used when optic neuritis is suspected.
Under the 2024 McDonald criteria, the optic nerves are one of the five regions considered when assessing dissemination in space, so optic nerve involvement can provide important clues to support an MS diagnosis.
Optic neuritis is commonly detected using optical coherence tomography, a noninvasive test that produces high-resolution images of the back of the eye to check for nerve damage.
Additional tests used to diagnose MS
A variety of other tests may be used to support the diagnosis of MS or exclude alternative explanations for symptoms. These may include:
- blood tests, to rule out infections, vitamin deficiencies, or autoimmune diseases, and measure MS-relevant biomarkers
- movement, coordination, and sensory tests, to detect problems that may result from damage to specific nerve pathways
- cognitive tests, to detect cognitive impairments that may arise in MS
- mood and mental health screenings, to look for depression and other emotional problems
Additional testing may be guided by a person’s specific symptoms. For example, if a patient experiences bladder issues, a urine test might be done to rule out other possible causes, while a colonoscopy or other digestive system exams may be considered if bowel problems are present.
| Test | Purpose |
|---|---|
| Blood tests | To exclude other possible causes of symptoms, such as infections |
| Movement, coordination, and sensory tests | To help detect problems resulting from damage to specific nerve pathways |
| Cognitive tests | To detect MS-related cognitive changes |
| Tests for emotional problems | To diagnose depression, anxiety, and other mental health issues |
Conditions to rule out in MS diagnosis
Before confirming an MS diagnosis, doctors must rule out conditions with similar manifestations. The differential diagnosis of MS may include:
- infections involving the CNS, including syphilis and Lyme disease
- other inflammatory and autoimmune diseases that can involve the CNS, such as lupus or vasculitis
- genetic disorders that can damage the myelin sheath, such as leukodystrophies or mitochondrial disease
- brain and spinal cord tumors
- migraine, especially with aura, which can cause temporary neurological symptoms and MRI changes that resemble those seen in MS
- damage to small vessels in the brain and other vascular conditions that can cause injury to myelin and nerve fibers
- certain deficiencies in vitamins and nutrients, such as copper or vitamin B12
- conditions that cause structural damage in the brain and/or spinal cord, such as a herniated disc
- other diseases characterized by CNS demyelination, including neuromyelitis optica spectrum disorder and acute disseminated encephalomyelitis
How long can MS go undiagnosed?
MS can go undiagnosed for several years, sometimes more than a decade, in part because early disease activity in the CNS can start years before symptoms are obvious. When symptoms do appear, they are often mild, intermittent, and nonspecific, so people may not recognize the need to see a doctor.
Delays may also occur if primary care doctors don’t immediately recognize symptoms as neurological and postpone referral to a neurologist, who is best equipped to diagnose MS.
Currently, most people are diagnosed within less than a year of symptom onset, but diagnostic delays are more common in people with atypical symptoms or a progressive disease course from onset.
How long does an MS diagnosis take?
Once MS is suspected, confirming the diagnosis can take weeks or months, although it can occasionally happen more quickly.
Waiting for referrals, consulting different specialists to rule out possible causes of symptoms, and undergoing various tests can all take time. For this reason, the time it takes to diagnose MS can vary significantly from person to person.
What is the average age of MS diagnosis?
Most people with MS are diagnosed between the ages of 20 and 50. However, a diagnosis can happen at any age, including in children and older adults.
Under the new diagnostic criteria, the framework for diagnosing MS is similar for children and adults, but doctors should request additional tests for children and older adults to reduce the risk of misdiagnosis.
Next steps after an MS diagnosis?
After an MS diagnosis is confirmed, patients and their healthcare providers should work together to develop an individualized MS treatment plan.
No two people are affected by MS the same way, and treatment decisions depend on disease type, symptom severity, lifestyle factors, and personal preferences. A patient may notice that their care needs change over time, so frequent and thorough communication will ensure that their needs are met at every stage of the disease.
Managing MS effectively requires a coordinated, multidisciplinary approach that brings together experts from various fields. A comprehensive MS care team focuses on these key areas:
- reducing disease activity and slowing MS progression
- treating relapses
- managing symptoms
- providing rehabilitation and mobility support
- offering emotional and mental healthcare
Beyond clinical treatment, lifestyle modifications like quitting smoking, exercising regularly, and maintaining a balanced diet play a vital role in managing MS symptoms and improving overall quality of life.
As a chronic disorder, MS requires ongoing monitoring. Patients should consult their neurologist regularly to assess the progression of their condition and its response to treatment, and adjust care as necessary.
Across the Multiple Sclerosis News Today website, patients can find information, support, and resources to get more familiar with the different aspects of the disease. People can also participate in forums to connect with others within the MS community and learn from the experiences of other patients through their shared stories and columns. Special content dedicated to those newly diagnosed with MS is also available.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

