Clinically isolated syndrome (CIS)
The presentation of multiple sclerosis (MS) varies between individuals, and doctors can’t always diagnose the disease after one episode of MS-like symptoms. A single episode of neurological symptoms suggestive of MS may initially be diagnosed as clinically isolated syndrome, or CIS, instead.
Abnormal immune attacks on the central nervous system (CNS), which includes the brain, spinal cord, and optic nerves, cause MS. These attacks target myelin, the protective sheath that covers nerve cells.
There are several types of MS, each with a distinctive clinical presentation and course. Most MS patients initially present with relapsing-remitting multiple sclerosis (RRMS), a form of the disease characterized by flare-ups or relapses where symptoms suddenly worsen, followed by periods of remission when symptoms ease and are generally stable. Sometimes, a second flare-up or other signs of disease activity are needed to confirm RRMS, and CIS may be a temporary diagnosis made after the first episode of neurological symptoms.
What is clinically isolated syndrome?
CIS is a first MS-like attack of neurological symptoms that:
- lasts at least 24 hours
- is caused by inflammation and myelin loss, or demyelination, in the CNS
- can’t be explained by other factors, such as fever or infections
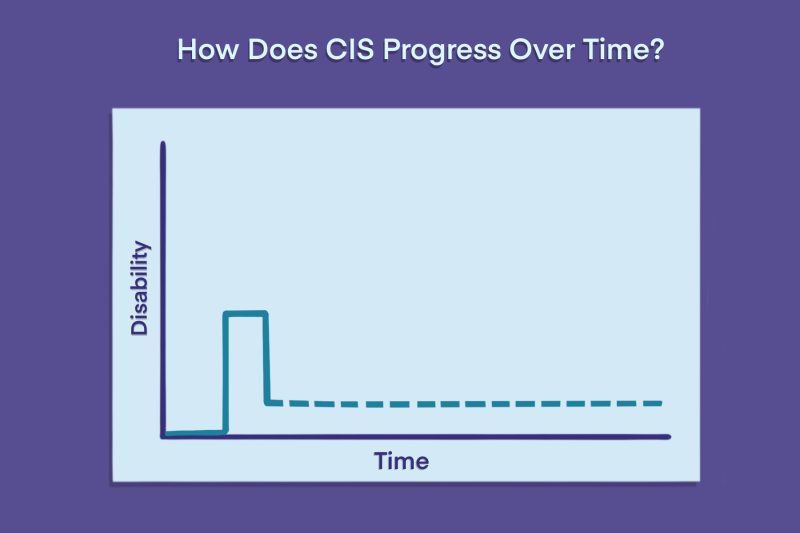
Usually, symptoms disappear partially or completely after the initial attack.
While a CIS diagnosis often precedes clinical confirmation of definite MS, it isn’t always an MS precursor. Some people with CIS don’t experience further symptoms and don’t go on to develop MS.
CIS can develop at any age, but it most commonly occurs in people between the ages of 20 and 40. It is two to three times more common in women than in men.
Symptoms of CIS
Every patient has a different experience with CIS, but symptoms are generally similar to those of an MS relapse. They may also resemble early warning signs or initial MS symptoms. Common CIS symptoms include:
- fatigue
- dizziness, vertigo, or nausea
- vision problems, including optic neuritis
- impaired cognition
If damage affects the spinal cord, symptoms of full or partial transverse myelitis, an inflammatory disorder, can also develop. These may include:
- numbness, tingling, or other abnormal sensations
- muscle weakness
- spasticity and muscle stiffness
- bladder and bowel problems
Physicians classify CIS as monofocal, meaning one symptom is present, or multifocal, meaning multiple symptoms are present. Typically, lesions, or areas of nerve cell damage, affect a single region of the CNS in monofocal disease, while multifocal CIS occurs when lesions affect several areas.
How long does CIS last?
Not all CIS patients will go on to be diagnosed with clinically definite MS, and the time until conversion to MS varies widely.
Historically, more than 60% of people with CIS have received an MS diagnosis in the first decade, and around 80% within 20 years of disease onset. However, estimates vary, with some indicating that around a third of people with CIS never develop MS within 30 years.
Several factors may affect CIS prognosis and the likelihood of developing MS. Notably, the chances of developing MS are greater in people with brain lesions at the time of their CIS diagnosis, with some studies indicating these patients have about an 80% chance of developing MS. Those with clear MRI scans have a 20% chance.
Individuals with CIS may have a higher risk of progressing to MS if they:
- are female
- were younger at the time of CIS onset
- are smokers
- have low vitamin D levels
- have more brain and spinal cord lesions on MRI scans
- test positive for markers of inflammation in the blood and spinal fluid
- present with certain disease symptoms, particularly fatigue, motor and cognitive impairments
Several disease-modifying therapies (DMTs) are available to help delay the progression to MS in people with CIS. However, the degree to which these modern therapies affect that transition isn’t entirely clear.
Diagnosis of CIS
There is no single test to diagnose CIS, or to confirm the progression from CIS to MS. The diagnosis process may involve several steps, including:
- evaluation of symptoms
- neurological examinations
- MRI scans to look for lesions in the brain and spinal cord, and identify characteristic features of the damaged areas
- a lumbar puncture to study the liquid that surrounds the brain and spinal cord (cerebrospinal fluid, or CSF)
These tests can help doctors find signs of CNS inflammation and demyelination, and rule out other potential causes of symptoms.
Recent changes in the formal guidelines used to diagnose MS, called the McDonald criteria, provided more pathways to a confirmed MS diagnosis after a single episode of MS-like symptoms.
Typically, a diagnosis of MS requires evidence of dissemination in time, meaning evidence indicating that neurological damage has happened at multiple points in time. Under the most recent guidelines, this is no longer necessary in certain cases when other supporting evidence is present, allowing MS to be diagnosed in some patients who have only experienced one episode of MS-like symptoms. This supporting evidence can come in the form of:
- MRI lesions in different parts of the CNS, or arising at different points in time
- signs of inflammation in CSF tests
- patterns typical of MS lesions
This means that some people previously diagnosed with CIS may now be diagnosed with clinically definite MS right away, even without having more relapses or recurring symptoms.
Treatment of CIS
In many cases, CIS symptoms are mild enough that patients don’t require immediate treatment. Many people recover entirely without any medications.
If symptoms are more severe or create substantial problems in everyday life, physicians may recommend glucocorticoids as a CIS treatment. These medications suppress inflammation and immune activity, potentially easing symptoms quicker.
CIS can’t be cured, but several DMTs may reduce the likelihood of experiencing new relapses or developing new brain lesions. They may also delay the progression of CIS to clinically definite MS or reduce the severity of later relapses.
However, because not all people with CIS will progress to have MS, the use of DMTs for CIS remains controversial. Patients and care teams should consider the likelihood of conversion to MS, potential risks and advantages of therapies, costs, and long-term treatment requirements when deciding whether to start a DMT.
Approved DMTs for CIS in the U.S. include:
- Aubagio (teriflunomide)
- Avonex (interferon beta-1a)
- Bafiertam (monomethyl fumarate)
- Betaseron (interferon beta-1b)
- Briumvi (ublituximab-xiiy)
- Copaxone (glatiramer acetate injection)
- Extavia (interferon beta-1b)
- Gilenya (fingolimod)
- Kesimpta (ofatumumab)
- Mayzent (siponimod)
- Ocrevus (ocrelizumab)
- Ocrevus Zunovo (ocrelizumab and hyaluronidase-ocsq)
- Plegridy (peginterferon beta-1a)
- Ponvory (ponesimod)
- Rebif (interferon beta-1a)
- Tascenso ODT (fingolimod)
- Tecfidera (dimethyl fumarate)
- Tyruko (natalizumab-sztn)
- Tysabri (natalizumab)
- Vumerity (diroximel fumarate)
- Zeposia (ozanimod)
Outlook of CIS
The prognosis of CIS varies broadly — some people will quickly progress to MS, while others may go decades without experiencing another attack or having evidence of new lesions.
CIS itself doesn’t affect life expectancy dramatically, with some studies indicating that patients may live for more than 45 years after first experiencing symptoms.
People with CIS should talk with their healthcare providers to develop a personalized treatment and care plan. In addition to DMTs, this may include medications to manage individual symptoms and lifestyle changes, such as adjusting diet, quitting smoking, or exercising appropriately.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

