Another Canadian Study Finds No Link Between Blocked Neck Veins And MS
Written by |
 Another study, in what has become a succession of Canadian studies, has failed to detect a link between blocked neck veins and multiple sclerosis proposed by Italian physician and researcher Dr. Paolo Zamboni in 2008 (a report in the Lancet noted that this hypothesis was originally posed by Putnam in 1947) that is termed “chronic cerebrospinal venous insufficiency” (CCSVI or CCVI). Dr. Zamboni also postulated that a vein-widening procedure, venous angioplasty, which he called “liberation treatment,” could improve the symptoms of MS patients.
Another study, in what has become a succession of Canadian studies, has failed to detect a link between blocked neck veins and multiple sclerosis proposed by Italian physician and researcher Dr. Paolo Zamboni in 2008 (a report in the Lancet noted that this hypothesis was originally posed by Putnam in 1947) that is termed “chronic cerebrospinal venous insufficiency” (CCSVI or CCVI). Dr. Zamboni also postulated that a vein-widening procedure, venous angioplasty, which he called “liberation treatment,” could improve the symptoms of MS patients.
Although there have been anecdotal claims of remarkable success resulting from CCSVI liberation treatment reported by some of the hundreds of MS patients who have sought the treatment, usually at substantial out-of-pocket expense or aided by fundraising efforts, for many others it has been an expensive disappointment for patients and their supporters. Wikipedia’s article on the topic notes that within the medical community, both the procedure and CCSVI concept itself have been met with skepticism, also observing that Dr. Zamboni’s first published research was neither blinded nor had a control group, and that Dr, Zamboni did not disclose his financial ties to Esaote, the manufacturer of the ultrasound specifically used in CCSVI diagnosis. Wikipedia reports that the “liberation procedure” has also been criticized for possibly resulting in serious complications and deaths while its benefits have not been proven.
The study published Monday in The Canadian Medical Association Journal, entitled “Validity of the diagnostic criteria for chronic cerebrospinal venous insufficiency and association with multiple sclerosis, (CMAJ June 2, 2014 First published June 2, 2014, doi: 10.1503/cmaj.131431), coauthored by  corresponding author Fiona Costello, M.D., Jayesh Modi, David Lautner, Deepak Bhayana, James N. Scott, W. Jeptha Davenport, Jessie Trufyn, Richard Frayne, Viesha A. Ciura, Mayank Goyal, Jean Mah, Michael D. Hill, variously of the Departments of Clinical Neurosciences (Costello, Modi, Scott, Davenport, Trufyn, Frayne, Ciura, Goyal, Hill), Surgery (Costello), Radiology (Modi, Lautner, Bhayana, Scott, Frayne, Ciura, Goyal), Pediatrics (Mah), Medical Genetics (Davenport), Medicine (Hill) and Community Health Sciences (Hill); Hotchkiss Brain Institute (Costello, Davenport, Hill); and Seaman Family Centre, Foothills Medical Centre, Alberta Health Services (Bhayana, Scott, Frayne, Goyal), at the University of Calgary, in Calgary, Alberta, found no link between a purported condition called chronic cerebrospinal venous insufficiency (CCSVI) and Multiple Sclerosis. after finding no difference in the proportion of abnormalities in the veins of MS patients and healthy controls.
corresponding author Fiona Costello, M.D., Jayesh Modi, David Lautner, Deepak Bhayana, James N. Scott, W. Jeptha Davenport, Jessie Trufyn, Richard Frayne, Viesha A. Ciura, Mayank Goyal, Jean Mah, Michael D. Hill, variously of the Departments of Clinical Neurosciences (Costello, Modi, Scott, Davenport, Trufyn, Frayne, Ciura, Goyal, Hill), Surgery (Costello), Radiology (Modi, Lautner, Bhayana, Scott, Frayne, Ciura, Goyal), Pediatrics (Mah), Medical Genetics (Davenport), Medicine (Hill) and Community Health Sciences (Hill); Hotchkiss Brain Institute (Costello, Davenport, Hill); and Seaman Family Centre, Foothills Medical Centre, Alberta Health Services (Bhayana, Scott, Frayne, Goyal), at the University of Calgary, in Calgary, Alberta, found no link between a purported condition called chronic cerebrospinal venous insufficiency (CCSVI) and Multiple Sclerosis. after finding no difference in the proportion of abnormalities in the veins of MS patients and healthy controls.
The coauthors observe that the chronic cerebrospinal venous insufficiency theory proposes that altered cerebral venous hemodynamics play a role in the pathophysiology of multiple sclerosis. We aimed to explore the validity of this hypothesis by assessing the diagnostic criteria for chronic cerebrospinal venous insufficiency in persons with and without multiple sclerosis.
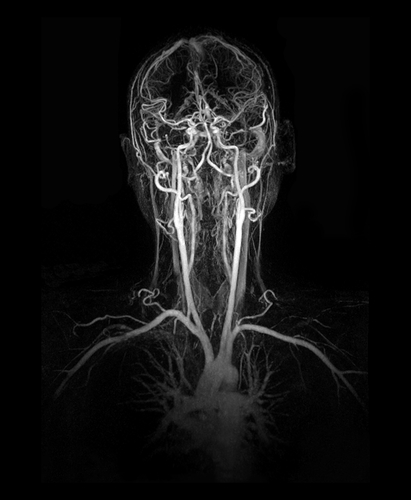
The U of A scientists compared the proportion of venous outflow abnormalities found in patients with multiple sclerosis with similar phenomena observed in healthy controls, using extracranial Doppler ultrasonography and gadolinium-enhanced magnetic resonance venography. Interpreting radiologists were blinded to the clinical status of participants.
Among the 120 patients enrolled with multiple sclerosis and 60 healthy controls, the researchers found high and roughly proportions of both MS patients (67/115 [58%]) and controls (38/60 [63%]) presenting with one or more of the proposed ultrasound criteria for diagnosis of chronic cerebrospinal venous insufficiency (p = 0.6). The researchers found that a minority of patients (23/115 [20%]) and controls (6/60 [10%]) fulfilled two or more of the proposed criteria (p = 0.1). There were no differences between patients and controls in prevalence of each individual ultrasound criterion. Similarly, there were no differences in intracranial or extracranial venous patency between groups, as measured by magnetic resonance venography.
[adrotate group=”4″]
The researchers conclude that there were no significant detectable differences in the proportion of venous outflow abnormalities between patients with multiple sclerosis and healthy controls. Moreover, their study revealed significant methodologic concerns regarding proposed diagnostic criteria for chronic cerebrospinal venous insufficiency that challenge their validity.
A study published in The Lancet last October entitled “Chronic cerebrospinal venous insufficiency in multiple sclerosis: the final curtain” (The Lancet, Volume 383, Issue 9912, Pages 106 – 108, 11 January 2014
doi:10.1016/S0140-6736(13)61912-1) by Friedemann Paul and Mike P. Wattjes also found that narrowing of the veins leading from the brain was found to be as prevalent in healthy individuals as it was in patients with MS.
 A commentary by New England Journal of Medicine Associate Editor Robert T. Naismith, MD notes that this study, along with other literature to date, convincingly supports no increase in prevalence in venous abnormalities for those with multiple sclerosis. Dr. Naismith observes that the Lancet study was well designed and included a large number of participants, careful blinding, standardized procedures, and direct comparison of venography with the more subjective and rater-dependent ultrasound technique, and cites an accompanying editorial contending that any additional research or healthcare dollars spent in pursuit of what the editorialist refers to as a misguided theory being money wasted, and that patients should be informed that there is no current evidence that venous angioplasty or stenting is beneficial in MS, and that the procedure includes small but undeniable risks.
A commentary by New England Journal of Medicine Associate Editor Robert T. Naismith, MD notes that this study, along with other literature to date, convincingly supports no increase in prevalence in venous abnormalities for those with multiple sclerosis. Dr. Naismith observes that the Lancet study was well designed and included a large number of participants, careful blinding, standardized procedures, and direct comparison of venography with the more subjective and rater-dependent ultrasound technique, and cites an accompanying editorial contending that any additional research or healthcare dollars spent in pursuit of what the editorialist refers to as a misguided theory being money wasted, and that patients should be informed that there is no current evidence that venous angioplasty or stenting is beneficial in MS, and that the procedure includes small but undeniable risks.
Sources:
The Canadian Medical Association Journal
The Lancet
New England Journal of Medicine
Wikipedia
Image Credits:
University of Alberta
New England Journal of Medicine


