ImStem Uses Embryonic Stem Cells to Treat Animal Model of Multiple Sclerosis
Written by |
 ImStem Biotechnology, Inc. is one step closer to harnessing the power of human embryonic stem cells (hESCs) to treat multiple sclerosis. Most recently, ImStem announced the successful treatment of an animal model of multiple sclerosis (experimental autoimmune encephalitis, EAE) using mesenchymal stem cells derived from hESCs (hES-MSCs).
ImStem Biotechnology, Inc. is one step closer to harnessing the power of human embryonic stem cells (hESCs) to treat multiple sclerosis. Most recently, ImStem announced the successful treatment of an animal model of multiple sclerosis (experimental autoimmune encephalitis, EAE) using mesenchymal stem cells derived from hESCs (hES-MSCs).
Using hES-MSCs to treat multiple sclerosis improves upon other researchers’ efforts of using bone marrow-derived MSCs (BM-MSCs), according to a paper published by ImStem in collaboration with University of Connect Health Center (UCHC) and Advanced Cell Technology, Inc., in Stem Cell Reports. “This was unexpected as BM-MSCs are widely believed to be effective in this EAE animal model. Our data indicate that the use of BM-MSCs is highly variable and there may be a previously unrecognized risk of poor outcome associated with IL-6 produced by these cells,” said Dr. Stephen Crocker from UCHC in a news release.
In reference to IL-6, this is a pro-inflammatory cytokine that, according to Dr. Xiaofang Wang of ImStem, “can worsen the disease.” Dr. Wang further explained that “BM-MSCs but not hES-MSCs express high levels of IL-6,” indicating why hES-MSCs are more efficacious in attenuating the neuroinflammation seen in multiple sclerosis. “The beauty of the new hES-MSCs is their consistently high efficacy in [this] multiple sclerosis model. This is a big surprise when we found that most BM-MSC lines show poor or no efficacy,” said Dr. Wang.
In the study, the group of researchers reproducibly generated MSCs from four different hESC lines and injected them into mice six days after immunizing the mice for EAE. To compare, the researchers also isolated MSCs from human donors and injected them similarly into other mice. The hES-MSCs delayed disease onset and reduced the daily, cumulative, and maximal disease scores of mice, but none of the BM-MSCs showed strong disease-inhibitory effects.
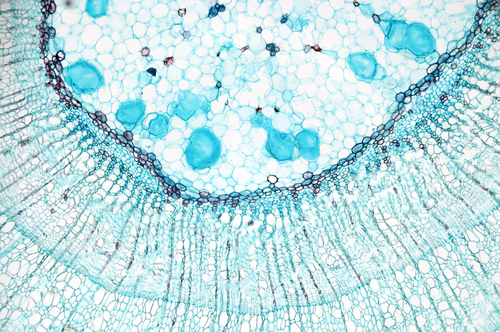
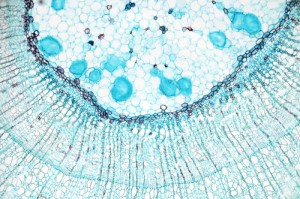
These results were attributed to a greater anti-inflammatory and lesser pro-inflammatory effect of hES-MSCs compared to BM-MSCs. Additionally, hES-MSCs were able to enter the inflamed tissue of the spinal cord, whereas BM-MSCs could only migrate to the spinal cord. “This difference is extraordinary as it could hold a key to the therapeutic actions(s) of hES-MSCs. MSCs might require access to specific sites within the central nervous system in order to remediate disease,” said Dr. Joel Pachter from UCHC.
[adrotate group=”4″]
Isolating MSCs from patient bone marrow can lead to a heterogeneous, poorly-defined mix of cells that are in short supply. Generating them from hESCs can be more well-defined, and the source is virtually unlimited. “These great advantages perfectly match the requirements for safety and quality control of clinical-grade MSCs as a potential therapy for autoimmune diseases such as multiple sclerosis, inflammatory bowel disease, and rheumatoid arthritis, said Dr. Ren-He Xu, CSO of ImStem.
Drs. Ren-He Xu and Xiaofang Wang founded ImStem in 2012. They were awarded a $1.13 million grant from the State of Connecticut Stem Cell Research Program and a $150,000 pre-seed fund from Connect Innovations in 2013. “Connecticut’s investment in stem cells, especially hESCs, continues to position our state as a leader in biomedical research,” said Governor Dannel Malloy. “This new study moves us one step closer to a stem cell based clinical product which could improve people’s lives.”


