Increased R&D Focus On PoNS Neuromodulation Therapy Device For People With MS; Other Neurological Conditions
Written by |

Newtown, Pennsylvania based Helius Medical Technologies, Inc. announced on June 6th that the company has entered into an agreement and plan of merger whereby the Company has agreed to acquire 100% of issued and outstanding common shares of Neurohabilitation Corporation (“Neuro”) of Delaware by way of a plan of merger.
Neuro, a medical device development firm, in January 2013 entered into an exclusive rights agreement whereby Advanced Neuro-Rehabilitation LLC (ANR) granted Neuro exclusive worldwide rights to ANR’s patents, trade secrets and knowhow, including a patent pending technology that will enable the first non-invasive means for delivering neurostimulation through the oral cavity — known as the “PoNs” stimulator.
The PoNS unit is a battery-powered device developed by three researchers at the University of Wisconsin Tactile Communication & Neurorehabilitation Laboratory (TCNL) scientists Yuri Danilov, Ph.D., Mitchell Tyler, M.S., P.E., and Kurt Kaczmarek, Ph.D. The PoNS sensor is placed in the mouth where thousands of nerve endings on the tongue can send messages to healthy areas of the brain. The concept is that lingual stimulation combined with therapeutic exercise, enables the brain form new neural pathways for recovering motor functions like balance and movement in persons affected by Multiple Sclerosis (MS), cerebral palsy, traumatic brain injuries, stroke, and Parkinson’s disease.
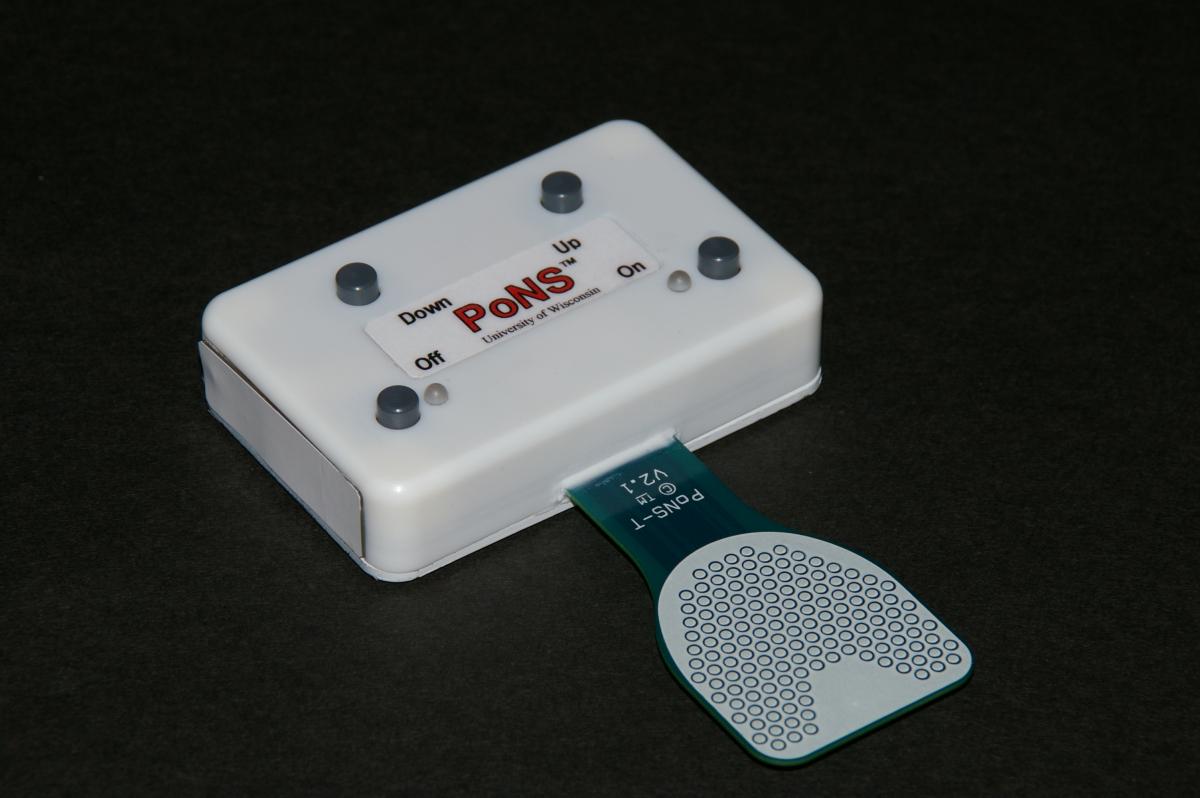
The PoNS is approximately 68 mm wide by 45 mm long by 15 mm thick and weighs approximately 56 grams. An oral tab on the T-shaped device provides the stimulation via 143 electrodes and fits on the anterior portion of the tongue, to be held securely in place by the lips. The PoNS device uses an unbalanced biphasic waveform designed to ensure net zero current to reduce chance of tissue irritation, and has 19 V max and 6mA operational limits. Pulses are delivered to the tongue in triplets of pulses at 5 ms intervals every 20 ms. The subject can control the pulse-width (0.4-0.6 s) by adjusting the intensity buttons on the device. The buttons on the device allow the stimulation to be turned on and off and increased or decreased in intensity. Each time the device is turned off, the intensity resets to the lowest level, requiring the subject to adjust it to a comfortable level each time (Kaczmarek, 2011). The device uses a rechargeable lithium-ion battery, and cannot be in use while charging to prevent risk of electrical shock. The tab, except for the electrodes, is covered with an FDA approved USP Class VI biocompatible polymer to prevent saliva from harming the electronics, and is cleaned with isopropyl alcohol after use. The price of the device, currently as a prototype, is approximately $5,000.
The brain’s ability to recognize its operation in response to new information sources, new functional needs, or new communication pathways is referred to as Nueroplasticity — a process that underlies all cerebral learning, training, and rehabilitation. Neuromodulation is the use of external tactile stimulation to intentionally change and regulate the internal electrochemical environment of the brain.
Interested in receiving more information about the PoNs stimulator for MS? Sign up for updates here!
[contact-form-7 id=”6518″ title=”Pons Device Contact Form”]
Traditional rehabilitation interventions have typically involved medication and various forms of therapies, including physical therapy, but the PoNS device is being investigated in combination with Physical Therapy for the treatment of Neurological symptoms from disease and trauma including traumatic brain injury (TBI) and MS.
The tongue has thousands of nerve fibers in it that help us eat, drink, and swallow. Without these nerve sensors, we would not taste. The tongue also allows us to speak, and quietly, its surface defends our bodies from germs. Another of the tongue’s most exciting roles is to serve as a direct “gateway” to the brain through thousands of nerve endings.
A TCNL study entitled “Cranial-nerve Non-invasive Neuromodulation (CN-NINM)” was conducted in collaboration with Professor Beth Meyerand of the UW Department of Medical Physics, and Professor Justin Williams in the UW Department of Biomedical Engineering, and funded by the University of Wisconsin Foundation via the TCNL Fund, has completed an initial program of research to explore the use of a new method of rehabilitation for neurological disease.
The study’s focus is to investigate conditions potentially treatable by CN-NINM, including initially movement disorders caused by stroke, traumatic brain injury, MS, and Parkinson’s disease, exploring the brain regions involved in CN-NIMM. The researchers are currently using two approaches: Functional magnetic resonance imaging (fMRI), and Electroencephalography (EEG).
Last year, the U.S. Army Medical Research and Materiel Command (USAMRMC) entered into a Cooperative Research and Development Agreement with NeuroHabilitation Corporation (NHC), a company formed by the TCNL co-directors in collaboration with TV personality Montel Williams — a military veteran who was diagnosed with multiple sclerosis in 1999, medical device specialist Jonathan Sackier, and Medimedia Health CEO Phil Deschamps. The Agreement allows the Army to work with NHC and TCNL to further develop and evaluate the PoNS device for use with soldiers who have experienced blast-related traumatic brain injuries.
Researchers at the U.S. Army Medical Research and Materiel Command in collaboration with UW-Madison and NeuroHabilitation Corporation are leveraging the power of those tiny nerves targeted restore lost physical and mental function for service members and civilians who suffered traumatic brain injury or stroke, or who have Parkinson’s or multiple sclerosis.
The treatment involves 20-30 minute stimulation therapy, called cranial nerve non-invasive neuromodulation, or CN-NiNM, using the PoNS device, and accompanied with a custom set of physical, occupational, and cognitive exercises, based on the patient’s deficits. The idea is to improve the brain’s organizational ability and allow the patient to regain neural control.
NeuroHabilitation Corporation, which was created with support by Montel Williams, funded initial commercial development of the device. A U.S. Army release notes that Mr. Williams was originally introduced to the PoNS research through an American Way magazine an attendant gave to him while he was on an American Airlines flight that contained an article about work being done at the University of Wisconsin-Madison. Shortly after reading the article, Mr. Williams joined a study at the University of Wisconsin-Madison’s Tactile Communication & Neurorehabilitation Lab of the Department of Biomedical Engineering.
“The third day there I said we need this in the mouths of our Soldiers,” Mr. Williams is cited stating, adding that he has always kept his ties with the military after serving in the Marine Corps and graduating from the U.S. Naval Academy.
Drs. Danilov, Tyler, and Kaczmarek’s research with the PoNS prototype at the TCNL is driven by the principle that brain function is not hardwired or fixed, but can be reorganized in response to new experiences, sensory input and functional demands.
[adrotate group=”4″]
The Army report notes that preliminary data from University of Wisconsin showed CN-NiNM to have great potential for a wide variety of neurological issues. Remarkably, the therapy doesn’t only slow functional loss, but also has the potential to restore lost function. That’s why researchers are saying that it “breaks the rules.” “When we talk about a brain changing itself, this is what we mean,” Dr. Danilov observes.
Because of its possible application for service members, especially those returning from combat with blast-related traumatic brain injuries, the USAMRMC signed a Cooperative Research and Development Agreement with NeuroHabilitation Corporation (founded by Williams and his colleagues, including the University of Wisconsin scientists), Feb. 8, that allows the Army to further evaluate the device.
“This exciting agreement leverages a unique private-public partnership,” commented Col. Dallas Hack, director of the USAMRMC Combat Casualty Care Research Program. “By collaborating with University of Wisconsin-Madison and NeuroHabilitation Corporation, we maximize our resources to explore a potential real-world treatment for injured service members and civilians with a variety of health conditions.”
Testing under the cooperative agreement includes a collaborative study with researchers and clinicians at the Blanchfield Army Community Hospital in Fort Campbell, Ky. as the result of a year-long coordination effort led by Capt. Ian Dews, deputy director of CCCRP. The hospital is home to the Warrior Resiliency and Recovery Center, which is dedicated to the treatment of Soldiers with physical and neuropsychological problems due to service-related trauma.
Additional patient testing is being conducted at other Veteran facilities and civilian medical institutions. Concurrently, the USAMRMC, in collaboration with its subcommands the U.S. Army Medical Materiel Agency and the U.S. Army Medical Materiel Development Activity, will conduct environmental testing, such as temperature and humidity limitations for the device, to better understand potential constraints. At the conclusion, the USAMRMC hopes to seek U.S. Food and Drug Administration clearance for PoNS.
The MS-Based Science Behind PoNS
Last July, a report entitled “Introduction To The Portable Neuromodulation Stimulator (Pons) Device And Effects On Balance And Gait For Individuals With Traumatic Brain Injuries” was presented at the Rehabilitation Engineering & Assistive Technology Society of North America (RESNA) Annual Conference at Bellevue, Washington, by Kati P. Liegl, Kathy L. Rust, and Roger O. Smith of the University of Wisconsin-Milwaukee’s Rehabilitation Research Design & Disability (R2D2) Center.
The project’s purpose was to introduce a new rehabilitation tool and the associated rehabilitation intervention (Cranial Nerve Non-Invasive Neuromodulation [CN-NINM]) on functional gait and balance for people with traumatic brain injuries. The study is intended to add to available research on the new intervention device and technique that may have significant effects on rehabilitation services.
The presenters noted that neurorehabilitation utilizes neuroplasticity of the brain to restructure and relearn information, typically after a neurotrauma. Individuals most commonly treated are those who have had a cerebral vascular incident, traumatic brain injury or spinal cord injury. Neurorehabilitation therapists use multiple techniques to help the patient improve, either by helping the patient relearn and improve previous skills, compensate with alternative techniques, or providing assistive technologies that may be temporary or permanently used. Neuromodulation alters the nervous system with the use of electricity or medications. Current, commonly used neuromodulation interventions include baclofen pumps, spinal cord stimulators, deep brain stimulators and transcranial magnetic stimulation. These interventions are not typically thought to have long lasting effects (Kern & Kumar, 2007; O Malley, Ro, & Levin, 2006), however, the effects noted during and directly after the application of the medication or electricity have substantial effects.
Participants in the study included individuals with vision impairments as well as with occluded vision. Electrical stimulation that provided the visual information was applied various places on the body, including the fingers, abdomen, back, forehead, and tongue. The tongue had the most favorable results for several reasons. The researchers note that the mouth provides a secure, discreet, and isolated environment for stimulation, maintains a relatively constant temperature and is not typically affected by environmental stimuli such as a breeze. Saliva maintains a constant pH+ and reduces the stimulation required for perception and interpretation. The tongue, because of the location and density of nerve receptors, requires less stimuli to respond than elsewhere on the body, including the fingers. In addition, participants have not indicated the sensation of the stimulation is unpleasant or painful (Bach-y-Rita & Kercel, 2003)
Liegl, Rust, and Smith observe that the CN-NINM neuromodulation technique, created at the University of Wisconsin-Madison in the Tactile Communications & Neurorehabilitation Laboratory (TCNL) has two primary components: 1) use of the Portable Neuromodulation Stimulator (PoNS) device to deliver small, safe doses of electric current to the tongue, and 2) targeted training activities that are personalized for each participant based on presenting symptoms and typically performed concurrently with the stimulation. The targeted maximal challenge training activities are similar to activities performed during standard neurorehabilitation but are additionally maintained for 20 minutes each to maximize neuroplastic effect. The researchers cite previous research using the PoNS device and CN-NINM intervention that have addressed impairments in balance and gait for several disability categories including traumatic brain injury, Parkinson’s disease, and stroke, among others.
A recent CN-NINM TBI withdrawal study published in the Journal of NeuroEngineering and Rehabilitation entitled “Non-invasive neuromodulation to improve gait in chronic multiple sclerosis: a randomized double blind controlled pilot trials” (J Neuroeng Rehabil. 2014; 11: 79. Published online May 1, 2014. doi: 10.1186/1743-0003-11-79 ) is coauthored by Drs. Danilov, Tyler, Kaczmarek, and Rust with Alla M. Subbotin and Kimberly L. Skinner of the Departments of Biomedical Engineering, and of Orthopedics and Rehabilitation, at the University of Wisconsin, Madison.
This study sought to examine the effect of targeted physical therapy with and without cranial nerve non-invasive neuromodulation (CN-NINM), on the walking ability of people with MS who exhibited a dysfunctional gait.
The researchers hypothesized that subjects who received electrical stimulation would have greater improvement than those who had a control device after a 14-week intervention. Gait disturbance is a common problem for people with MS. Management may include exercise, pharmacology, functional electrical stimulation, compensatory strategies, use of assistive devices, and implanted electrical devices, which have been combined with rehabilitative strategy using neuromodulation of the cranial nerves via electrical stimulation of the tongue to enhance the plasticity of the brain.
[adrotate group=”4″]
In the within-subject blinded randomized control design study, twenty chronic MS subjects with an identified gait disturbance were assigned to either an active or control group. Both groups completed a 14-week intervention program using a standardized combination of exercise and a device that provided electrical stimulation to the tongue. Those in the active group received electrical stimulation on the tongue that they could perceive. Those in the control group used a device that did not provide a physiologically significant stimulus and was not perceivable. Subjects were assessed with the Dynamic Gait Index (DGI).
The researchers report that while DGI scores improved for both groups, there were significant between-group differences, with the active group showing statistically greater improvement than the control group mean, leading to the conclusion that people with MS demonstrated improved gait with CN-NINM training in this pilot randomized controlled trial. Subjects who trained using exercise only without stimulation (control group) continued to improve for the first month at home and then exhibited a plateau or even a decrease in performance, providing preliminary evidence that the intervention is effective when performed independently at home. Because the tongue stimulation device is portable, it allows people to train at home, affording an therapeutic model not previously reported. This leads the scientists to speculate whether people with other types of neurological conditions would benefit from this type of intervention to improve motor control.This study also suggests that tongue-based neurostimulation may amplify the benefits of exercise for improving gait in people with chronic MS, although the coauthors note that the sample size of this study was small (10 subjects per group), which may limit the external validity of the results.
It remains undetermined whether CN-NINM training could be practically deployed in a rehabilitation setting, since the in-lab training for this study was time intensive (approximately 2 to 3 hours per day, per subject), involving far more time for therapy than a typical clinical setting would allow. This was an intentional departure from most therapeutic models for rehabilitation, derived from the researchers’ prior experience with treating vestibular disorders. Given the rigors of the intervention, and the nature of this neurodegenerative disease, this intensive in-lab phase was designed to ensure that subjects understood and could reliably perform the training program before using the device at home. However, they contend that the results suggest that this new paradigm for home-health rehabilitation, particularly for disorders previously deemed untreatable, is efficacious, and additional studies are warranted to determine if an abbreviated intervention would be as effective as the model presented in the report, an to investigate the breadth of applicability that this form of therapeutic intervention may have for meaningful neurorehabilitation.
A controlled study of people with mild to moderate traumatic brain injuries (mTBI) begins this month, investigating if balance problems and other symptoms resulting from a TBI will improve with cranial nerve non-invasive neuromodulation (CN-NINM). This intervention, to be conducted at the University of Wisconsin, Madison campus at the Tactile Communication and Neurorehabilitation Lab, will use therapeutic exercises combined with simultaneous electrical stimulation on the tongue via the PoNS device.
Persons eligible for participation in the study will be between the ages 18 and 65, have experienced a mild or moderate closed-head TBI, have difficulty with balance and walking, be at least one year post-injury; and able to walk for at least 20 minutes. Other entrance criteria wil apply.
Participants will be asked to spend two weeks at the University of Wisconsin in Madison for initial training, which includes exercises in balance, walking, movement, and relaxation, and takes approximately three hours per day.
Subsequently they will continue training at home for 12 weeks, approximately two hours per day, returning to the UW for weekly appointments during the 12-week home training period, and every 3 weeks for appointments for a second 12-week period (the withdrawal phase).
Compensation will be up to $600 for participation in this study.
For more information, visit:
https://tcnl.bme.wisc.edu/node/95
For more information on the PoNS device, visit:
https://www.universaldesignstyle.com/pons-device-promising-technology-for-ms/
Sources:
The University of Wisconsin
University of Wisconsin Tactile Communication & Neurorehabilitation Laboratory (TCNL)
U.S. Army Medical Research and Materiel Command
Rehabilitation Engineering & Assistive Technology Society of North America (RESNA)
Journal of NeuroEngineering and Rehabilitation
Helius Medical Technologies, Inc.
NeuroHabilitation Corporation
UniversalDesignStyle
Image Credits:
University of Wisconsin Tactile Communication & Neurorehabilitation Laboratory (TCNL)
U.S. Army Medical Research and Materiel Command