JCV Virus May Be Missed in Patients Who Take Popular MS Drug, According To Study
Written by |

 Multiple sclerosis (MS) patients who are prescribed Tysabri have an increased risk to develop the rare, often fatal infection of the brain called progressive multifocal leukoencephalopathy (PML), according to a recent study. PML is caused by a common virus that infects blood cells and can be mobilized by popular RRMS drug Natalizumab, which is known by its brand name Tysabri. Furthermore, the study revealed that some MS patients who have the virus may be unaware, as current tests have been found to miss the infection.
Multiple sclerosis (MS) patients who are prescribed Tysabri have an increased risk to develop the rare, often fatal infection of the brain called progressive multifocal leukoencephalopathy (PML), according to a recent study. PML is caused by a common virus that infects blood cells and can be mobilized by popular RRMS drug Natalizumab, which is known by its brand name Tysabri. Furthermore, the study revealed that some MS patients who have the virus may be unaware, as current tests have been found to miss the infection.
The study, entitled, “JC Virus in CD34+ and CD19+ Cells in Patients With Multiple Sclerosis Treated With Natalizumab,” appeared in a recent issue of JAMA Neurology. According to study author Eugene Major, a senior investigator at the US National Institute of Neurological Disorders and Stroke (NINDS) in Bethesda, Maryland, around one in seventy-five MS patients who have been treated with Tysabri for two years or more and who have also been prescribed additional immune-suppressing drugs go on to show positive results for the PML virus.
What makes PML particularly dangerous in that the typically benign John Cunningham virus (JCV) associated with the infection attacks the fat wrappings or myelin in the brain, effectively removing the insulation function around the axons of nerve cells. Once this insulation is destroyed, neurons have difficulty sending action potentials and lose their ability to communicate to other cells. As the disease progresses, MS patients experience weakness, paralysis, impaired vision, slurred speech, and cognitive problems. NINDS reports that 30 to 50 percent of PML patients die after only a few months after being diagnosed, and those that survive may have permanent disability.
Interestingly, the majority of people have JVC, however, the more serious PML is rare. The infection presents in individuals who have suppressed or compromised immune systems, such as those who have HIV/AIDS or patients taking an immunosuppressant drug such as Tysabri.
Researchers report that three factors identified in the recent study appear to put Multiple Sclerosis individuals at the highest risk for PML: taking Tysabri therapy for two years or more, taking other immunosuppressant medications, and a positive test revealing JCV antibodies in the blood.
[adrotate group=”4″]
Tysabri has a checkered past. The FDA first approved it in late 2004, but was quickly taken off the market after only three months specifically because a high rate of PML cases began to crop up in clinical trials. The drug was eventually allowed back on to the market in 2006 with stricter prescribing conditions and an increased awareness of the potential for the drug to give rise to PML infections. Specifically, in 2010, the FDA added a warning label to Tysabri regarding the increased risk of PML. Since then, this subject has continued to be a topic of conversation in the medical community, with JAMA Neurology publishing an observation related to the issue, entitled, “Lessons Learned From Fatal Progressive Multifocal Leukoencephalopathy in a Patient With Multiple Sclerosis Treated With Natalizumab,” published in March of 2013.
To determine why Tysabri carries a PML risk in MS patients, in the recent study, researchers analyzed two Multiple Sclerosis patient groups’ blood samples. One group had just started Tysabri therapy, and the second group had been taking Tysabri for over two years. These samples were compared to healthy volunteers.
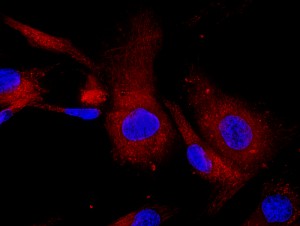
What researchers looked for was evidence of stem cells that turn into B-cell lymphocytes. Major notes in the study that, “. . . in these MS patients treated with [Tysabri], the number of these blood stem cells is three- to 10-fold higher than you’d see normally under normal physiologic conditions. The JC virus is able to infect these blood stem cells as they become a B lymphocyte.” He believes that these infected B cells then carry infection into the brain. To test his hypothesis, Major and colleagues set out to see if they could find traces of the JCV in circulating blood stem cells.
Out of the 26 patients who had just begun taking Tysabri, 50 percent were found to have traces of JCV in samples of their blood stem cells. Out of the 23 patients who had been taking Tysabri for two years or more, 44 percent presented with JCV DNA found in multiple blood stem cell types. Furthermore, Out of the 18 healthy volunteers used as control subjects in the study, only 17 percent of them showed signs of JCV in their blood cells.
Major notes, “It was somewhat surprising to us that quite a high percentage of individuals had detectable viral DNA in these blood stem cells.” However, it is not clear as to how this could affect their risk of developing PML. Most of the patients who tested positive for JCV had only a few copies of the virus which suggests that they were still at low risk of infection. Major suggests, “We need to look at additional patients, and follow them for a long period of time.”
What concerned researchers most was that 10 participants had evidence of JCV in their blood but tested negative for antibodies. This suggests that current tests may be missing some patients who could be at high risk for PML.


