NIH Study into Progressive MS Biomarkers to Be Presented at ACTRIMS 2016
Written by |
Scientists from the Neuroimmunological Diseases Unit at the National Institutes of Health (NIH) will present results of a study investigating several biomarkers that might lead to a more sensitive and accurate diagnostic test of central nervous system (CNS) inflammation, a key aspect of progressive multiple sclerosis (MS).
The data is being reported today, Feb.18, at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum 2016 by NIH researcher Dr. Mika Komori. The presentation, titled “Combination of biologically related biomarkers quantifies infiltration of CNS tissue by immune cells in progressive multiple sclerosis,” will be given in Session 1, “Emerging Concepts in MS.”
Progressive MS is usually divided into two stages: primary progressive MS (PPMS) and secondary progressive MS (SPMS), which follows relapsing-remitting MS (RRMS) as a new disease phase. Both PPMS and SPMS patients exhibit progressive disability and fewer magnetic resonance imaging (MRI)-detected brain lesions, leading to a general understanding that little inflammation in progressive MS is caused by autoimmunity. Rather, its symptoms and overall CNS tissue destruction are likely a consequence of neuronal and axonal degeneration. Results from several clinical trials support these assumptions, and immunomodulatory drugs are known to fail progressive MS patients, despite being effective in those with RRMS.
The research team’s goal was to develop a more reliable method of detecting and measuring CNS inflammation and immune cell infiltration, as current methods and biomarkers are not sensitive enough to detect low to moderate levels of inflammation or distinguish between PPMS and SPMS.
Researchers collected and examined the cerebrospinal fluid (CSF) of 198 participants, patients diagnosed with RRMS, PPMS, SPMS, non-inflammatory neurological disorders (NIND), and other inflammatory neurological disorders (OIND), and a group of healthy donors (HD). All samples were quantified for 19 soluble biomarkers and CSF immune cells, used to determine three different ratios of CSF biomarkers’ concentration and corresponding CSF cells (B cells, T cells and monocytes) per milliliter of CSF.
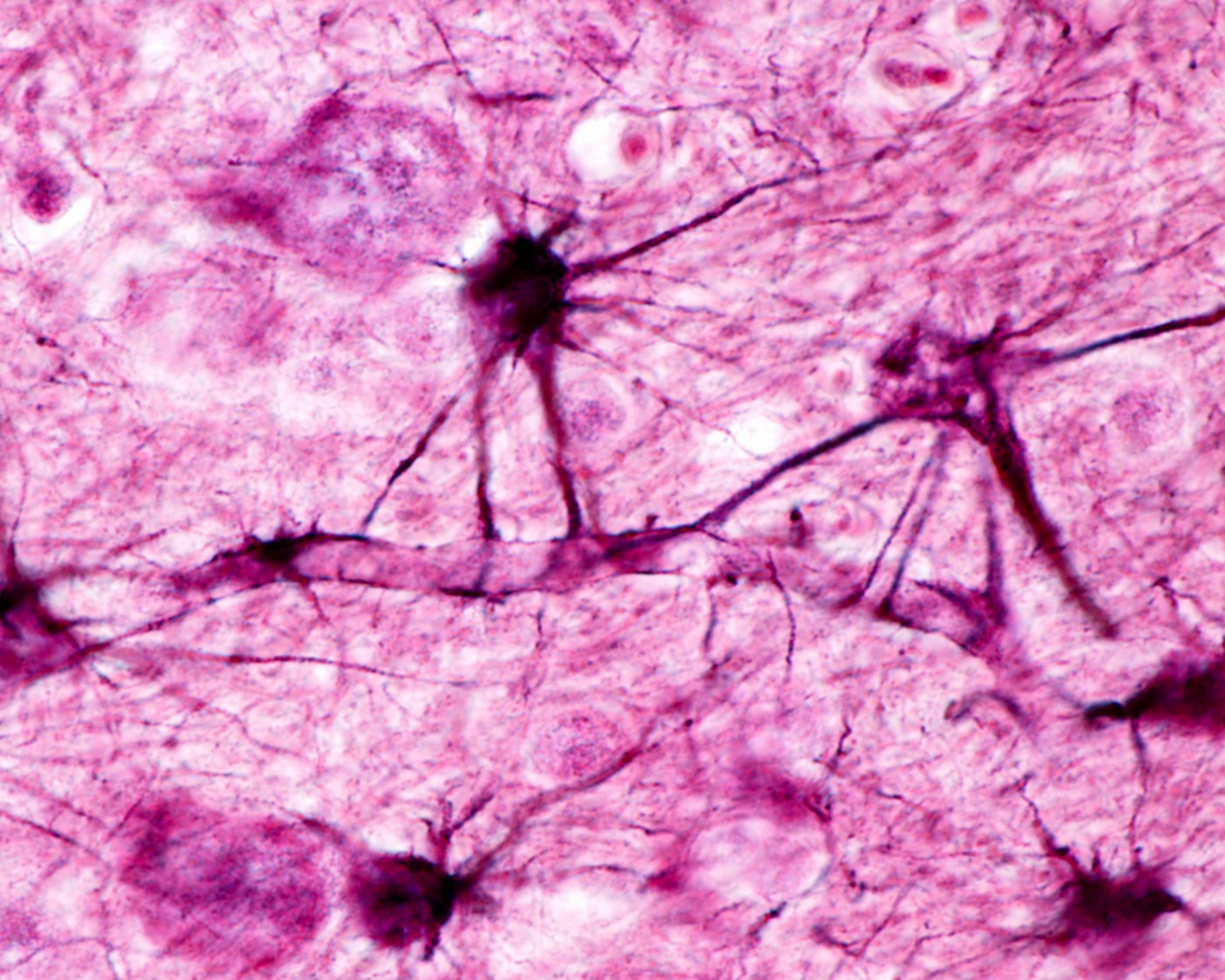
Ratios relating specifically to biomarkers of B and T cells (sCD21/B-cell and sCD27/ T-cell ratios) were found to be significantly higher in progressive MS than in all other disease groups, distinguishing progressive MS from RRMS. The excess of soluble biomarkers in relation to the number of cells is interpreted as an indicator of the presence of non-mobile cells within the CNS tissue, an interpretation that was further validated by available CNS autopsy/biopsy results.
“Intrathecal levels of T and B cells in progressive MS are comparable to RRMS. The major difference is that while in RRMS the immune cells are mobile, in progressive MS they are predominantly embedded in CNS tissue. This compartmentalization of the immune responses is likely the major reason for the failure of current immunomodulatory treatments in both subtypes of progressive MS,” the researchers concluded in their ACTRIMS’ abstract.


