Fingolimod (Gilenya) Seen to Promote Peripheral Nerve Regeneration in Mice, Aiding Remyelination
Written by |
Fingolimod (Gilenya), a drug approved for patients with relapsing-remitting multiple sclerosis (RRMS) to prevent neuroinflammation, may also help these patients by directly enhancing nerve regeneration and increasing myelination in a way that is partly independent of its anti-inflammatory properties.
The study reporting this finding, “Fingolimod promotes peripheral nerve regeneration via modulation of lysophospholipid signaling,” was developed by researchers at the Medical Faculty, Heinrich-Heine-University, in Germany, and published in the Journal of Neuroinflammation.
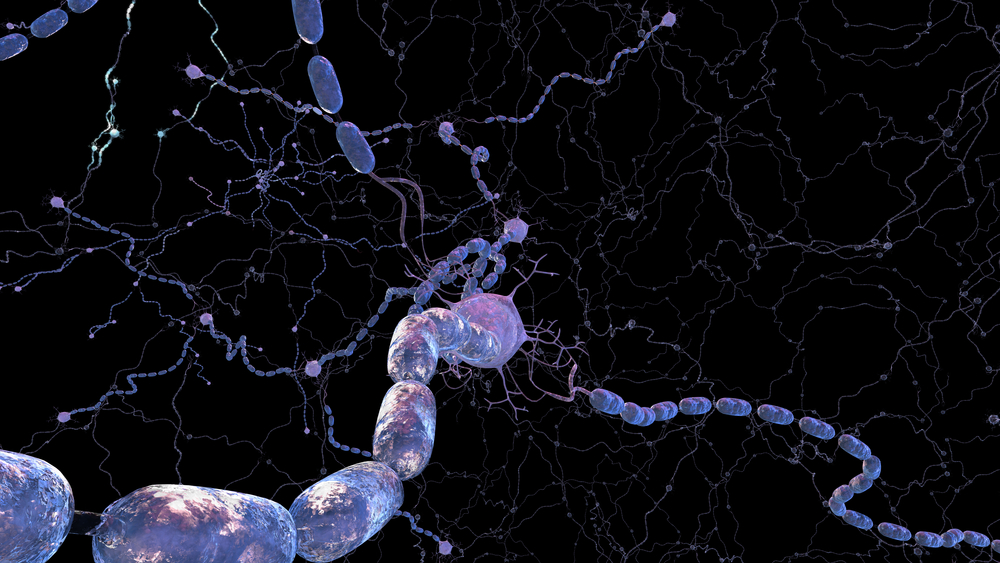
Sphingosine-1-phosphate (S1P) is a lysophospholipid known to have a critical role in the immune system. It binds to the receptor S1P1, expressed in lymphocytes, inducing lymphocyte migration from the lymph nodes into broader circulation. Fingolimod is a S1P receptor agonist that binds to the S1P receptors and shuts down their signaling, preventing lymphocyte spread and reducing neuroinflammation by decreasing the amount of immune cells in the central nervous system.
Fingolimod has also demonstrated an ability to act as an inhibitor of autotaxin, an enzyme that generates a lysophospholipid called lusophosphatidic acid (LPA). In turn, LPA seems to be associated with damage to brain tissue, and has been implicated in nerve demyelination. Fingolimod is consistently reported to promote functional recovery in models of spinal cord injury, but its effects on nerve cells is not well-known.
Researchers in Germany investigated the lymphocyte-independent effects of fingolimod on peripheral nervous system regeneration. The team performed sciatic nerve crush, a widely accepted model for studying peripheral nerve regeneration, and analyzed fingolimod’s effects in normal mice, mice lacking T-cells, and mice depleted of both immune B- and T-cells.
Results showed that nerve regeneration following fingolimod treatment was partly independent of the drug’s anti-inflammatory properties, as only mice with B-cells responded to treatment. Fingolimod use induced high levels of cAMP, a molecule involved in a number of signaling pathways in the axons, which is crucial for axon growth.
The authors believe that B-cells are required for this process because they clear myelin debris, which often contains inhibitors of axonal growth by reducing the levels of neuronal cAMP.
Furthermore, the research team found that fingolimod decreased LPA levels in an injured nerve, most likely by autotaxin inhibition, which improved myelin thickness. In fact, when the autotaxin-specific inhibitor PF-8380 was used, myelin thickness was strikingly similar to that observed before nerve injury.
But PF-8380 treatment did not lead to signs of improved axonal regeneration, which suggests that fingolimod has a dual role of action in peripheral nerve regeneration.
“In addition to the established role of fingolimod as a modulator of S1P receptor-mediated signaling, the inhibition of LPA synthesis after injury may represent a yet unrecognized mechanism that contributes to the presumptive remyelinating effect of fingolimod,” the authors concluded in their study.


