Fat Bubbles and Ultrasound May Offer Way of Getting MS Therapies Directly to Brain
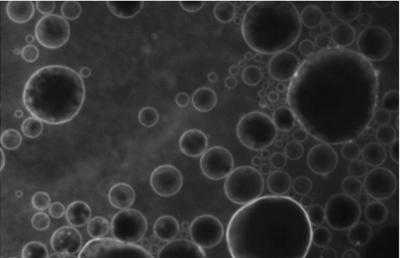
Microbubbles. (Credit: UEIL, Columbia University, C. Sierra et al.)
A new ways of delivering drug therapies directly to the brain, overcoming the limitation imposed by the blood-brain barrier (a permeable barrier that protects the brain), has been discovered. The technique — which makes use of lipid bubbles and ultrasound — may pave the way for new treatments against neurological disorders, including multiple sclerosis (MS).
The study describing the method, “Lipid Microbubbles As A Vehicle For Targeted Drug Delivery Using Focused Ultrasound-Induced Blood-Brain Barrier Opening,” was published in the Journal of Cerebral Blood Flow and Metabolism.
The blood-brain barrier works to select which molecules can enter the brain and which cannot. It necessarily protects the brain from pathogens circulating in the blood, such as virus, bacteria or fungi, but this barrier’s lock also extends to drugs that could help treat neurological disorders such as MS, Parkinson’s and Alzheimer’s.
Several approaches have been developed over the years to try to get around the barrier, but few has been effective in opening the barrier momentarily to allow a drug treatment through. It currently blocks 98 percent of available treatments arriving by bloodstream, reacting to them as pathogens. The importance of delivering a treatment directly to affected brain regions is of immense importance, because it might allow for treating those region without affecting other organs.
Physicist Carlos Sierra and colleagues at Columbia University in New York have developed a novel way to overcome the barrier and deliver drugs directly into the brain. The method consists in an intravenous injection of drug molecules that are first embedded in microbubbles made of lipids (fat). Researchers then use ultrasound (like a laser) to release the microbubbles into the specific brain area where they are needed. The ultrasound, pointed at the brain area, makes the microbubbles oscillate and increase in size as they arrive there. When they reach a certain size (8 microns), they rupture and open the blood-brain barrier, allowing the drug to enter the brain.
“We’ve made a step forward by incorporating the substance we’re interested in into the lipid coating of the microbubbles,” said Sierra, in a news release. “This makes the substance stay adhered to the microbubbles and prevents it circulating freely through the body.”
With the initial injection, drug molecules can be found throughout the body, but these molecules will travel to the brain, where the ultrasound stimulates their release from the microbubbles. “It does all this, while being non-invasive, reversible and completely safe,” Sierra added.
The team demonstrated the technique’s efficacy on mice, using a fluorescent dye to track the location of the carrier microbubbles under a microscope and made sure they were delivered to the brain area chosen. Researchers also identified certain ultrasound parameters for using this delivery system in a living being.
According to Sierra, more studies need to be carried out before the technique may be tested in patients, but he believes it may “be applied to diseases like Parkinson’s, Alzheimer’s, Huntington’s diseases, brain tumours, strokes, multiple sclerosis and amyotrophic lateral sclerosis, where we expect to see a very significant rise in the efficacy of treatment and a considerable reduction in side-effects.”
The team is currently testing its efficiency in the delivery of a drug therapy for Parkinson’s, and have obtained promising preliminary results.
“[T]he success of this technique in mice, and even in monkeys, can’t guarantee it will be effective in people, but if we continue to get satisfactory results then pre-clinical trials on humans would begin,” Sierra concluded.






