Blocking Protein, Reelin, Seen to Protect Immune System From Inflammation
Written by |
Lowering levels of a protein called reelin — which regulates how permeable blood vessels are to immune cells — reduced infiltration of these cells into the central nervous system (CNS), preventing neuroinflammation and disease progression in a mouse model of multiple sclerosis (MS).
These data, which also showed that Reelin is present at higher-than-normal levels in MS patients during relapses, support Reelin as a potential new therapeutic target for MS. Nevertheless, further studies are needed to confirm the potential benefits of this approach in MS and other inflammation-related conditions, the researchers noted.
“We think we can use this intervention for a wide range of inflammatory diseases that have been difficult to therapeutically address,” Joachim Herz, MD, the study’s senior author, said in a University of Texas Southwestern Medical Center (UTSW)’s press release.
The study, “Reelin depletion protects against autoimmune encephalomyelitis by decreasing vascular adhesion of leukocytes,” was published in the journal Science Translational Medicine.
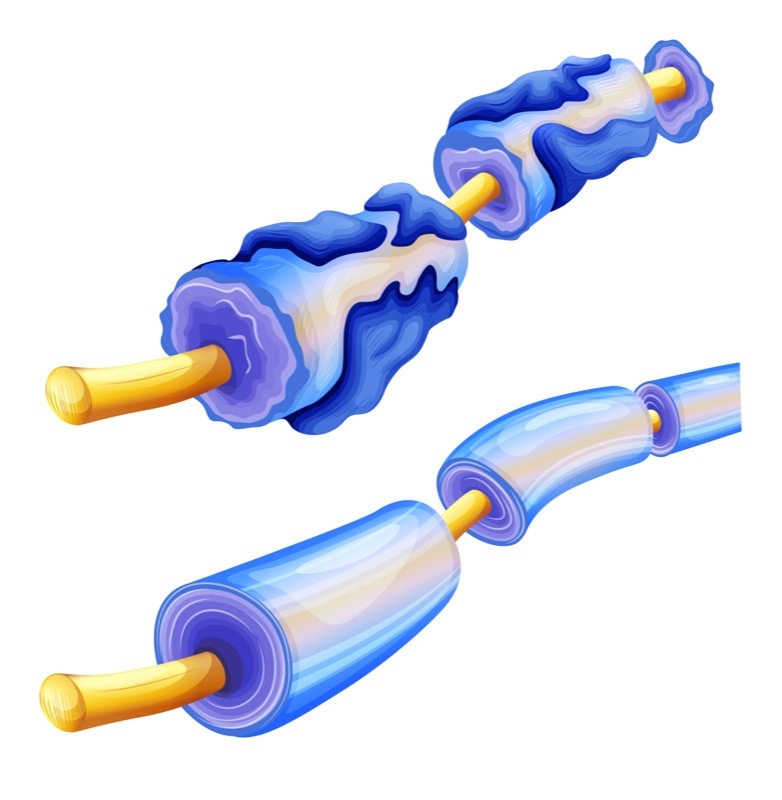
In MS, circulating immune cells infiltrate the CNS (the brain and spinal cord), where they wrongly attack myelin, the protective sheath that covers nerve fibers, and promote inflammatory reactions that eventually cause nerve cells to die.
Various therapies for MS, approved or in development, aim to prevent immune cells from infiltrating the CNS so to halt neuroinflammation, demyelination (loss of myelin), and disease progression.
However, serious side effects are known with most of these approved therapies, highlighting a need for better and safer immunomodulatory approaches.
Researchers at the UTSW, along with a colleague at Reelin Therapeutics, identified a potentially safer way of preventing immune cell infiltration in MS by targeting a protein called reelin.
Initially identified for its role in brain development, and neural connections during adulthood, reelin was more recently reported to act on endothelial cells (those lining blood vessels), regulating the adhesion and passage of monocytes — a type of inflammation-inducing immune cell — to and through the endothelium.
Notably, a mutation in RELN, the gene that contains the instructions to produce reelin, was also found to be associated with MS severity and age of onset.
To assess whether reelin could be contributing to immune cell infiltration and MS progression, the team first analyzed reelin blood levels in 43 people with relapsing-remitting MS, in remission (24 patients) or during an acute relapse (19 patients), and 18 healthy individuals.
Patients during relapse had significantly higher levels of reelin compared with those in remission, who showed similar levels to those found in healthy people, the researchers found.
This suggested that “circulating Reelin correlates with MS severity and stage,” they wrote.
Further analyses in both human and mouse endothelial cells confirmed that blocking reelin with a selective neutralizing antibody suppressed immune cell adhesion to endothelial cells.
The team then evaluated the effects of lowering reelin levels in mice with experimental autoimmune encephalomyelitis (EAE), an established animal model of MS.
Results showed that dropping reelin levels in these mice, either through the genetic deletion of RELN or using a reelin-neutralizing antibody, suppressed the ability of monocytes to attach to endothelial cells, preventing their entry into the CNS.
This was associated with lesser neuroinflammation, demyelination, and paralysis severity, when comparing with non-treated EAE mice.
Antibody-mediated reduction in reelin levels also showed protective effects in mice already displaying symptoms of the disease, highlighting the potential benefits of this approach in treating MS patients.
Overall, the findings established “an alternative endothelial-specific tunable immunomodulatory approach for the treatment of MS by selectively reducing endothelial permeability and infiltration of inflammatory cells into the CNS,” the researchers wrote.
They noted that such approach is likely to have a good safety profile, as it selectively targets immune cells’ endothelial adhesion, while avoiding direct immune cell suppression.
Besides MS, other chronic inflammatory conditions that depend on excessive immune cell endothelial passage, such as atherosclerosis, arthritis, or Crohn’s disease, may also benefit from this approach, the researchers suggested.
“We are now in the process of testing this in animal models for these human diseases,” said Herz, adding that the team is also working to develop a reelin-neutralizing antibody “that can clear Reelin from human blood.”
Both Herz and Laurent Calvier, PhD, the study’s first author, are shareholders of Reelin Therapeutics and co-inventors of a patent related to anti-reelin strategies.


