#MSVirtual2020 – Lesions First Seen on Nerves of GI Tract in Mouse Model of MS
Written by |
Before signs of neurodegeneration in the brain and spinal cord are evident in mice with experimental autoimmune encephalomyelitis (EAE) — which resembles human multiple sclerosis (MS) — signs can first be found in the network of nerves innervating the gastrointestinal (GI) tract, a study reports.
Additional research is needed to confirm these findings, its investigators stressed.
Still, these results add to the growing body of literature supporting the importance of this network of GI nerves in the onset and development of neurodegenerative diseases, including amyotrophic lateral sclerosis, Parkinson’s, and Alzheimer’s disease as well as MS.
Findings were detailed at MSVirtual2020 by Stefanie Kürten, MD, PhD, with the Institute of Anatomy and Cell Biology at Friedrich-Alexander University Erlangen-Nürnberg in the oral presentation, “The Enteric Nervous System as a Potential Autoimmune Target in Multiple Sclerosis.”
In MS, the fatty sheath of myelin protecting nerve endings is gradually destroyed by the immune system, leading to the formation of lesions in the central nervous system (CNS; the brain and spinal cord).
However, more than 60% of MS patients report experiencing GI problems, and more than 30% claim these symptoms start before the onset of the disease itself, challenging the notion that MS is restricted to the CNS.
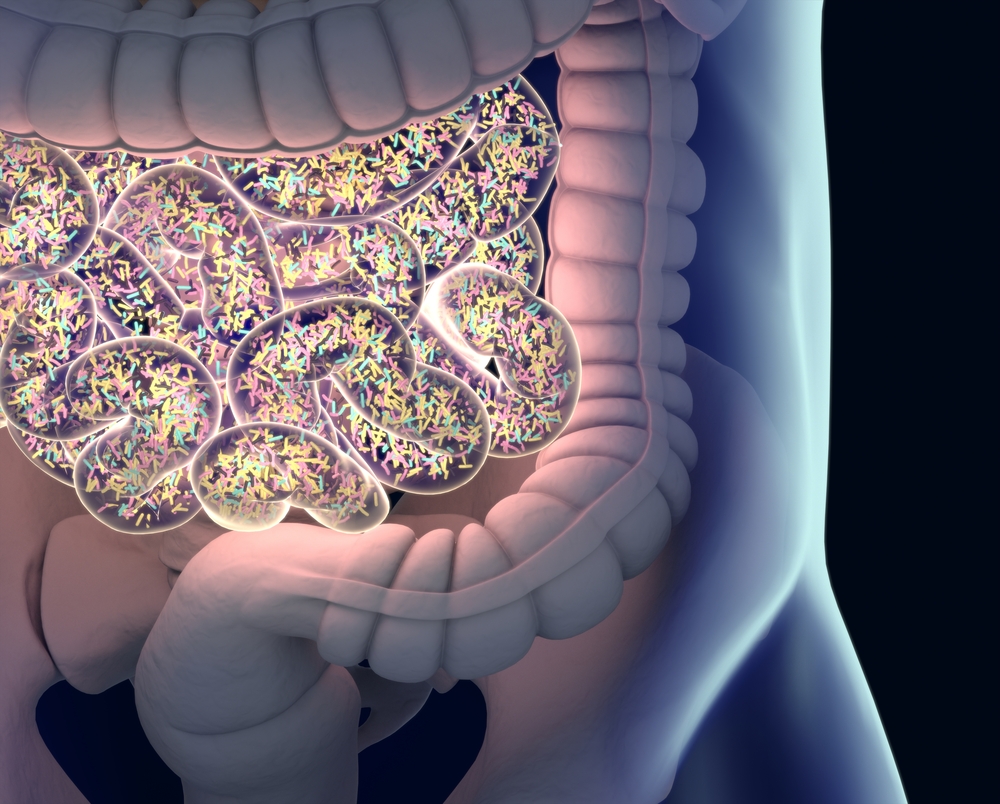
To test if the network of GI tract nerves — known as the enteric nervous system (ENS) — could actually be affected before the CNS, researchers examined the ENS of mice with EAE, a well-established animal model of MS.
Using a combination of different tissue labeling techniques and high-resolution imaging microscopy, they discovered that the animals’ ENS started showing signs of neurodegeneration before CNS lesions appeared.
This was particularly striking in the myenteric plexus, a component of the ENS that innervates the muscles surrounding the GI tract.
“The myenteric plexus looks completely destroyed [in these animals],” Kürten said during the presentation. “You hardly have any healthy axons remaining and … the muscle layer looks heavily atrophic [muscle atrophy or loss].”
Of note, axons are the long nerve fibers responsible for transmitting electrical signals between nerve cells.
Functional analyses revealed that the formation of these lesions in the animals’ ENS was accompanied by poorer GI transit.
Enteric nervous system lesions in these animals were also seen to be caused by self-reactive antibodies targeting myelin components, such as myelin basic protein (MBP) and proteolipid protein (PLP), similar to the process seen in the CNS, the researchers reported.
When these investigators examined portions of the colon taken from MS patients during surgery, they found evidence of local inflammation and neurodegeneration in the nerves forming the myenteric plexus, similar to what they had seen in the mice.
“Our current working hypothesis is that in the context of … EAE you will have the formation of both MBP and PLP specific antibodies. These antibodies then go on to bind to not only to the CNS, but also to the ENS … and as a result the ENS will degenerate,” Kürten said.
Additional studies are needed to confirm if neurodegeneration truly occurs in the ENS before appearing in the CNS, Kürten said.
However, “this is very difficult to do in MS patients themselves. We are going to use our [mouse] model to address this question,” she added.
The team is also examining samples from MS patients to determine if different types of neurons found in the ENS may be targeted and affected by these self-reactive antibodies differently.
Studies are also underway to “address the question whether there are cross-reactivity with foreign antigens [molecules able to induce an immune response], in particular with food components, and antigens of the central nervous system and the enteric nervous system,” Kürten said.
Here, Kürten emphasized a particular ongoing project in which the team is analyzing the role of cow milk in MS. A previous study suggested a correlation between the consumption of liquid cow milk (as opposed to dairy products like cheese) and MS prevalence.
The team believes there might be cross-reactivity between cow milk’s protein casein and different myelin antigens present in both the CNS and ENS, potentially aggravating symptoms in MS patients who consume unprocessed cow milk.


