PML caused by Tysabri results in lasting neurological symptoms
Most disability progresses without disease relapses, inflammatory activity

People with multiple sclerosis (MS) who develop progressive multifocal leukoencephalopathy (PML) as a side effect of Tysabri (natalizumab) often see their neurological symptoms worsen severely during the infection and their disability gradually accumulate over time.
That’s according to a study in Austria, which also showed that most disability progression following the rare brain infection occurred in the absence of disease relapses or inflammatory activity in the brain.
There have been fewer cases of PML in recent years, but the data “emphasize that [PML] represents a devastating disorder that must be avoided at all costs,” the researchers said in “Long-term outcome of natalizumab-associated progressive multifocal leukoencephalopathy in Austria: a nationwide retrospective study,” which was published in the Journal of Neurology.
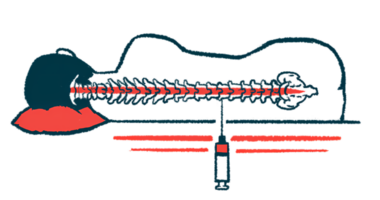
Marketed by Biogen, Tysabri is an antibody-based therapy for relapsing forms of MS, where episodes of new or worsening symptoms, called relapses, are followed by periods of recovery. It works by blocking a protein that helps white blood cells move out of blood vessels and into the brain and spinal cord, where they drive inflammation and contribute to MS. By blocking it, Tysabri reduces the resulting inflammation, easing disease activity and slowing the accumulation of MS symptoms.
Long-term effects of PML with Tysabri
While it’s highly effective at controlling MS, Tysabri is known to increase the risk of PML, a rare but serious brain infection caused by the John Cunningham virus.
This risk is highest among patients who’ve been on Tysabri for more than two years or have received immunosuppressants, and for those who test positive for antibodies against the John Cunningham virus.
Because the infection can be life-threatening or result in severe disability, there are strict requirements in most countries for monitoring patients on Tysabri. This ensures prescribers are aware of its risk and are able to detect and control PML when it becomes evident.
Researchers in Austria reviewed medical records at the Austrian MS Treatment Registry and MS centers across the country to get a better understanding about what happens over the long term to someone who’s developed PML on Tysabri. They identified 15 patients (67% women) who were a median age of 40 and had MS for about a decade when were diagnosed with PML.
The participants had received a median 52 infusions of Tysabri and only one patient had been receiving it for less than two years. The researchers noted that 80% of PML cases occurred between 2010 and 2015, and only three occurred after 2016, “when increased vigilance commenced.”
After a median follow-up of 76 months, three patients died, an overall mortality rate of 20%. Two patients died about two months after the diagnosis due to immune reconstitution inflammatory syndrome (IRIS), a state of very severe inflammation. The third died five years later, although the cause was considered to be related to the fulminant neurologic damage he experienced during the infection.
Increased disability levels with PML infection
Disability levels were measured with the Expanded Disability Status Scale (EDSS), whose scores range from 0, indicating no disability, to 10, for death. While the clinical course after PML varied between patients, EDSS scores increased from a median of 3.5 points before PML to 6.5 points after the infection.
In this period, seven (47%) patients saw severe disability progression and five (33%) saw their EDSS scores increase by 3 points or more. Six patients developed seizures, which “were exclusively observed among patients with a severe EDSS increase on long-term outcome,” the researchers wrote.
Most patients (55%; six of 11) continued to have worsening disability in the long term, compared with measurements taken after the PML infection had resolved. Four patients remained stable and one improved.
“Many patients had accumulated severe persistent neurological deficits at long-term follow-up, which was however mostly related to the EDSS changes associated with the acute PML phase,” the researchers wrote, noting during follow-up that one patient had one relapse and another had evidence of disease activity on MRI scans. “Besides one single clinical relapse recorded, signs of inflammatory MRI activity were observed in one other individual,” they wrote.
Three (20%) patients went on to develop secondary progressive MS, a more severe form of the disease that usually follows relapsing-remitting MS.
While the number of cases of PML appears to be “decreasing over time,” in part due to “risk mitigation strategies” and fewer patients being treated with Tysabri, PML “was associated with severe persistent neurological deficits in the majority of cases,” said the researchers, who called for more research.