Intrathecal methotrexate halts disability worsening, data show
Most in small trial see stable disability levels over time
Written by |
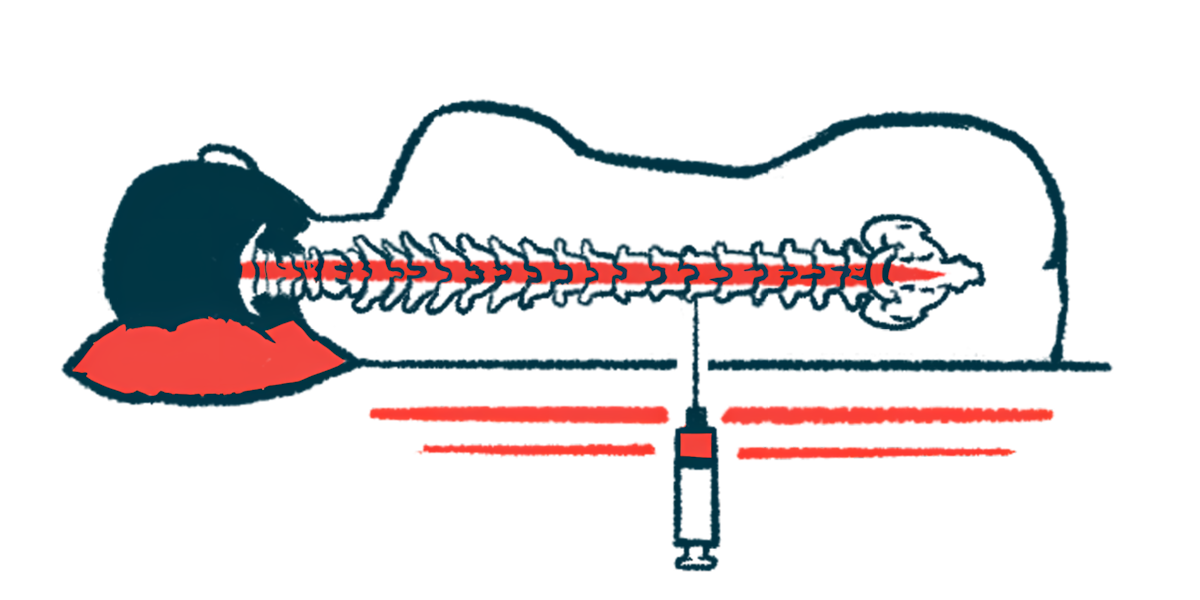
Injections of methotrexate into the spinal canal given every three months were safe and well tolerated, and helped adults with progressive forms of multiple sclerosis (MS) maintain stable disease levels for up to nine years.
That’s according to data from a small, open-label Phase 1 clinical study (NCT02644044) that tested how safe and well tolerated intrathecal methotrexate is and how well it works to slow disability worsening in people with primary or secondary progressive MS.
The study, “Intrathecal methotrexate in progressive multiple sclerosis: a phase 1 open-label study with long-term follow-up,” was published in the Journal of Neurology.
In MS, the immune system mistakenly attacks myelin, a sheath that that covers nerve cells and helps them send electrical signals more efficiently. While a number of therapies are approved for relapsing forms of MS, fewer options exist for people with progressive forms of the disease, particularly from those who don’t experience any relapses.
“There is still an unmet need for effective treatments for progressive forms of the disease,” the researchers wrote.
Benefits in other autoimmune diseases
Methotrexate is an anti-cancer medication that may help slow disability worsening in MS by reducing inflammation in the brain and spinal cord. It works by interfering with the normal production of immune cells. The therapy has been widely used in other autoimmune diseases, and has been tested in relapsing and progressive forms of MS with some promising benefits.
The researchers set out to investigate the safety and efficacy of methotrexate in progressive MS given as an intrathecal injection instead of via infusions into the bloodstream. They conducted an open-label Phase 1 trial involving 22 patients — 10 with primary progressive MS and 12 with secondary progressive MS — who had experienced disability worsening in the past six months but had no relapses or active inflammatory lesions in that period.
Participants’ average age was 57.6, and they had been living with MS for about 13.1 years. They were treated with intrathecal methotrexate every three months for one year.
The long-term safety and efficacy of treatment was assessed in a group of 10 patients who continued on methotrexate after completing the Phase 1 trial or who were not part of the trial but declined to receive or discontinued treatment with Ocrevus (ocrelizumab) upon its approval. These patients received treatment for 2-9 years.
Methotrexate was given at a dose of 12.5 mg. Patients also received dexamethasone, a corticosteroid, to reduce the risk of side effects from the intrathecal injection.
The main goal was to watch for changes in disability levels, as measured with the Expanded Disability Status Scale (EDSS), the 25-Foot Walk (25FW), and the Symbol Digit Modalities Test (SDMT), after one year. 25FW measures walking function, while SDMT is frequently used to assess cognition.
In the six months prior to the study, the median EDSS score increased from 5.5 points to 6.5 points, indicating worsening disability. However, no significant changes were observed after six months and one year on methotrexate. In fact, more than two-thirds of patients had stable or improved EDSS scores after six months (72.7%) and after one year (68.2%).
Similarly, no significant changes were seen in 25FW and SDMT scores at six months and one year. Of the 20 who completed the first six months of treatment, only 30% had disability progression in one of the three clinical measures, while 30% had disability improvement in one measure over the same period.
Most patients tolerated the treatment well. The most common side effect (for 32%) was headache after the lumbar puncture. Serious side effects, including vomiting and dehydration that required hospital admission, were reported in two patients.
In the longer follow-up, patients received methotrexate for a median of 4.2 years. During that period, seven patients experienced no changes in their EDSS scores, indicating stable disability levels, while three saw increases of 0.5 points. No serious side effects were reported over a combined treatment duration of 44 years.
The findings show that short- and long-term use of intrathecal methotrexate is safe and well tolerated, with most patients maintaining stable disability levels.
“These findings support [intrathecal methotrexate] as a promising therapeutic approach for [progressive MS], particularly for patients progressing despite approved disease-modifying therapies or unable to tolerate them,” the researchers wrote. “Further large-scale studies are warranted to confirm these results.”


