No MS disability progression for over 60% after stem cell transplant
UK study finds better results after 5 years in RRMS vs. progressive MS
Written by |
Nearly two-thirds of people with multiple sclerosis (MS) who underwent a stem cell transplant showed no signs of confirmed disability progression five years later, according to a study tracking MS patients in the U.K.
The results were generally better for people with relapsing-remitting MS (RRMS), but nearly half of individuals with progressive forms of the neurodegenerative condition also remained free of disability progression after five years, the data showed.
While some safety issues were reported, these were generally more common in people with more advanced disease or those who had received higher chemotherapy dosages before the transplant.
Those findings, the researchers noted, highlight the critical importance of carefully selecting patients for stem cell transplant and optimizing treatment protocols to maximize safety and long-term benefits.
The study, “Autologous haematopoietic stem cell transplantation for multiple sclerosis in the UK: A 20- year retrospective analysis of activity and haematological outcomes from the British Society of Blood and Marrow Transplantation and Cellular Therapy (BSBMTCT),” was published in the journal Transplantation & Cellular Therapy.
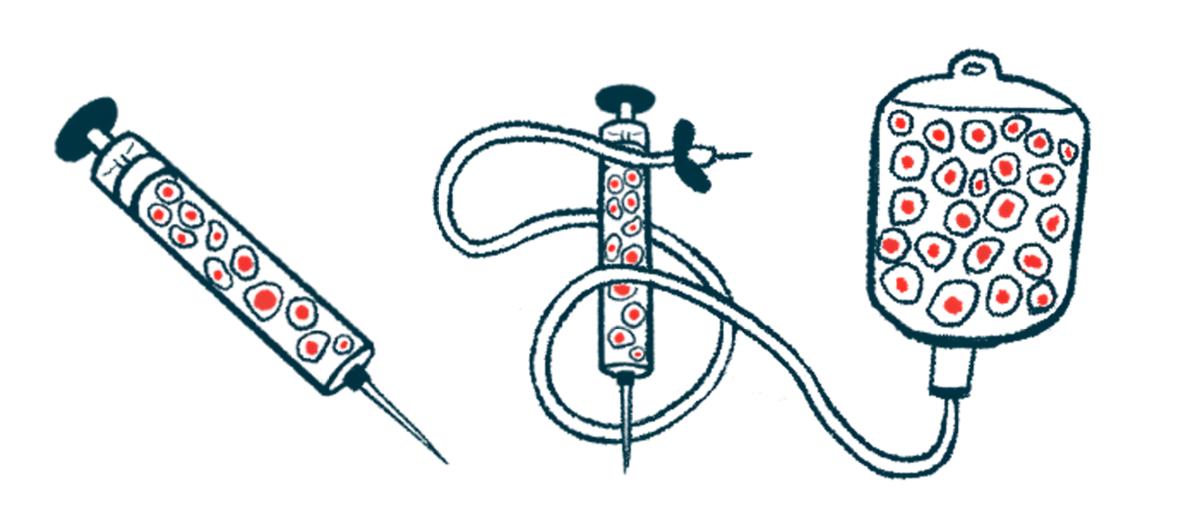
Autologous hematopoietic stem cell transplant (aHSCT), also referred to as stem cell therapy, is a procedure designed to reset the immune system and reduce the excessive inflammation that drives MS.
It involves collecting a patient’s stem cells from their bone marrow or blood, followed by an intensive conditioning chemotherapy regimen to partly or completely ablate the immune system and eliminate the faulty immune cells. The stored stem cells are then infused back into the patient to rebuild a normally functioning immune system.
Assessing real-world efficacy of stem cell transplants in MS
aHSCT has been proven more effective than standard disease-modifying therapies (DMTs) in achieving no evidence of disease activity (NEDA), a status in which patients experience no relapses, no worsening disability, and no new lesions.
However, it is often considered a high-risk treatment. While mortality rates have dramatically decreased since the 1990s, when it was first used to treat MS, “safety concerns and lack of awareness still restrict AHSCT access,” the researchers wrote.
In the U.K., for example, aHSCT has been available for MS patients since 2013 through the National Health Service (NHS). However, fewer than 0.3% of potentially eligible patients have undergone the procedure. Also, comprehensive national data on outcomes are lacking, the team noted.
To better understand the U.K. patient experience with aHSCT in real-world practice, the research team examined data from 364 people with MS who received a transplant in one of 14 centers in Great Britain from 2002 to 2023.
Slightly more than half of the patients (58%) had RRMS, while 36% had been diagnosed with either primary progressive MS (PPMS) or secondary progressive MS (SPMS). A total of 6% had no known disease type. At the time of the transplant, the patients had a median age of 40, and most had severe disability, with a mean score on the Expanded Disability Status Scale (EDSS) of six points.
Nearly all patients (98%) received conditioning with a combination of cyclophosphamide, a chemotherapy drug, and rabbit anti-thymocyte globulin (rATG), and an immune-suppressing medication. The rest (2%) received a stronger chemotherapy regimen.
Outcomes best for RRMS patients, with no progression for 68%
All patients had successful engraftment of their stem cells, meaning the transplanted stem cells homed in on the bone marrow and began producing new blood cells. This occurred at a median of 11 days after the transplant, data showed.
Early complications were common, occurring in 97% of patients. This most often was fluid overload, where excess fluid builds up in the body, causing swelling or breathing problems, clinically significant fluid retention or weight gain, and high-grade fever during conditioning.
In the first 100 days after aHSCT, five patients (1.4%) died, mostly due to conditioning-related toxicity. Three more patients died more than a year after transplant, but these deaths occurred due to disease progression, COVID-19, or unknown causes, according to the researchers. At the time of the transplant, these patients all had significantly advanced disease, the study noted.
[Stem cell transplant] remains a very effective one-off therapy for treatment of patients with severe MS. … Careful patient selection by a multidisciplinary team is important to optimise risk/benefit, and data collection is vital for meaningful ‘real-world’ outcome analysis.
A few other safety issues were also reported after treatment with aHSCT. These included new cancers (1.6%), new new autoimmune conditions (7.9%), and viral reactivations (76%), particularly of the Epstein-Barr virus (EBV).
“Viral reactivation, particularly EBV, remains a significant issue and routine monitoring is mandatory for the first 100 days,” the researchers wrote.
Regarding efficacy, 62% of patients remained free from confirmed disability progression five years post-transplant. Outcomes were best in RRMS, with 68% of patients experiencing no sustained progression of EDSS scores compared with 59% of those with SPMS and 46% of PPMS patients.
The researchers noted that patients who received lower doses of rATG (6 mg/kg or lower) were more likely to remain progression-free from 90 days post-transplant onward, particularly those with RRMS. In contrast, those who experienced viral reactivation had poorer long-term outcomes.
“In conclusion, AHSCT remains a very effective one-off therapy for treatment of patients with severe MS,” the researchers wrote. “Careful patient selection by a multidisciplinary team is important to optimise risk/benefit, and data collection is vital for meaningful ‘real-world’ outcome analysis.”


