Human Gut Microbes May Help Suppress MS, New Research Suggests
Written by |
A bacteria present in the gut, called Prevotella histicola, prevented multiple sclerosis (MS) from developing in a preclinical mouse model, found researchers at the Mayo Clinic in Rochester, Minnesota, along with colleagues at the University of Iowa.
Their study, “Human Gut-Derived Commensal Bacteria Suppress CNS Inflammatory and Demyelinating Disease,” appeared in the journal Cell Reports.
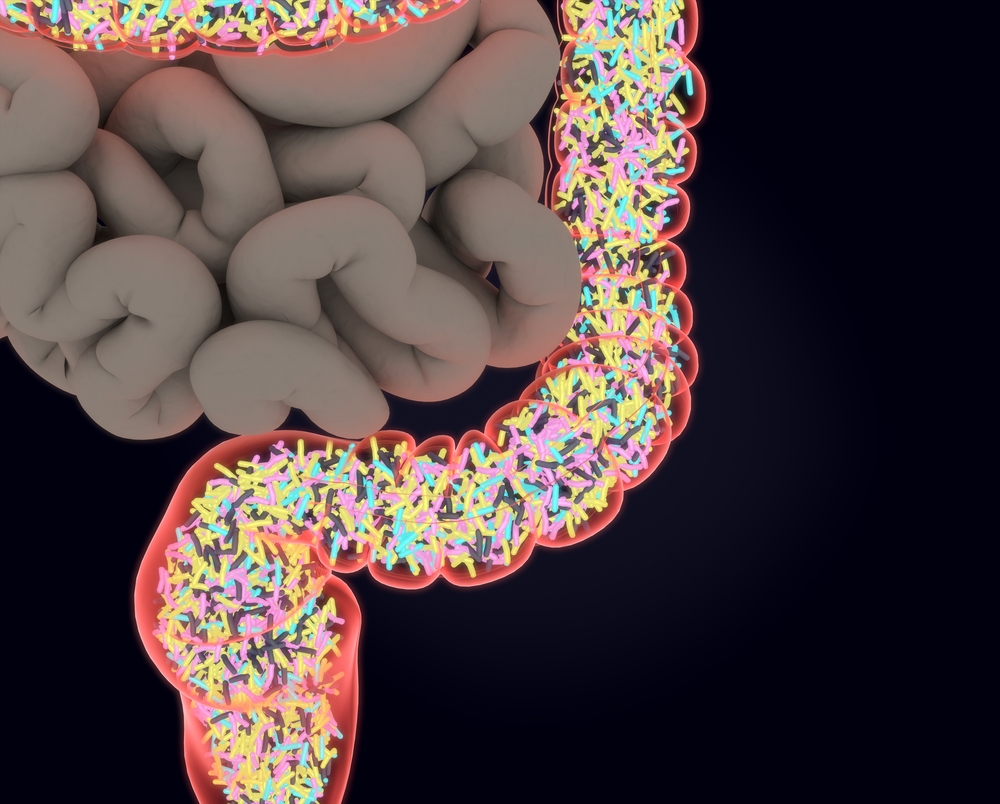
Current research suggests that alterations to the gut microbiome residing in human intestines may potentially trigger inflammatory diseases such as MS. In an attempt to identify which gut resident bacteria are capable of modulating immune responses, researchers studied cultured small pieces of intestine tissue extracted from biopsies of patients with celiac disease.
The team then isolated three bacteria strains and found that one of species — P. histicola — had the capacity to suppress MS in a preclinical animal model of the disease.
“This is an early discovery but an avenue that bears further study,” Dr. Joseph Murray, a Mayo Clinic gastroenterologist and the study’s lead author, said in a press release. “If we can use the microbes already in the human body to treat human disease beyond the gut itself, we may be onto a new era of medicine. We are talking about bugs as drugs.”
By investigating how P. histicola modulated immune responses to suppress MS, researchers found that bacteria decreased the expression of two pro-inflammatory cytokines – interferon-gamma and interleukin (IL)-17. Overall results show that P. histicola has immune modulatory activity and can suppress abnormal immune responses, which ultimately prevent autoimmunity. This supports the idea that maintaining a healthy microbial community within our intestines is a potential therapeutic strategy for MS.
“Our work is a classic example of a bedside-to-bench and potentially back to bedside study. Recent MS microbiome studies have shown the lack of Prevotella genus in patients with the disease and an increase when patients were treated with disease-modifying drugs,” said Ashutosh Mangalam, the study’s first author and an assistant professor of pathology at University of Iowa’s Carver College of Medicine. “And it’s not just for MS, because this may have a similar modulating effect on other nervous system and autoimmune diseases.”


