#MSParis2017 – GNbAC1 Promotes Restoration of Protective Myelin Coating, Phase 2b Trial Shows
Written by |

GeNeuro‘s humanized antibody GNbAC1 promotes the rejuvenation of the myelin coating that protects nerve cells in patients with relapsing-remitting multiple sclerosis, or RRMS, a Phase 2 clinical trial shows.
The treatment is also safe, the study showed.
Dr. Hans-Peter Hartung of the Heinrich-Heine-University Düsseldorf in Germany presented the results at the 7th Joint ECTRIMS-ACTRIMS Meeting in Paris, Oct. 25-28. The presentation was titled “Week 24 results from a Phase IIb trial of GNbAC1 in patients with relapsing remitting multiple sclerosis (CHANGE-MS; Clinical trial assessing the HERV-W Env antagonist GNbAC1 for Efficacy in MS).”
The research dealt with the retrovirus underpinnings of some of our DNA. Researchers believe up to 8 percent of our genome — or full set of DNA, including all of our genes — consists of retroviral DNA. This is DNA altered by the remnants of ancient retroviral infections. Scientists call the remnants human endogenous retroviruses, or HERVs.
Growing evidence suggests that activating HERVs contributes to inflammatory processes, and consequently to diseases like MS. In fact, a protein known as pHERV-W Env is common in inflammation patches known as lesions in MS patients’ brains, and in their blood.
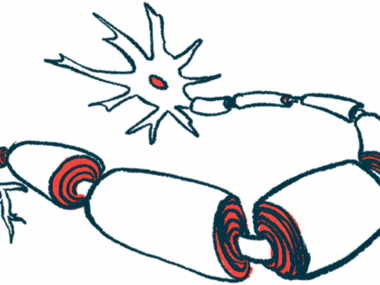
The lesions are areas where myelin, a protein that protects nerve cells, has deteriorated. Loss of myelin is a hallmark of MS.
PHERV-W Env protein promotes inflammation and prevents cells known as oligodendrocyte precursor cells from restoring myelin in the brain lesions that have lost it.
GNbAC1 is a humanized IgG4 antibody that blocks the pHERV-W Env protein’s pro-inflammatory effects and promotes remyelination. GeNeuro studied GNbAC1 in three completed Phase 1 and 2a clinical trials before conducting the Phase 2b study that Hartung discussed.
The Phase 2b CHANGE-MS study (NCT02782858) looked at GNbAC1’s effectiveness in 270 RRMS patients ages 18 to 55.
GeNeuro conducted the trial at several centers in Europe. Researchers randomly assigned patients to one of three doses of GNbAC1 or a placebo. Participants received monthly intravenous infusions of their treatments for 24 weeks.
After that, patients who had received a placebo were re-randomized to receive one of the three doses of GNbAC1 for an additional 24 weeks.
The trial’s primary objective was to see if NGbAC1 reduced the number of patients’ brain lesions, compared with lesions in the placebo-treated group. Researchers used magnetic resonance imaging brain scans between weeks 12 and 24 to make this determination.
One of the trial’s secondary objectives was to see whether NGbAC1 reduced patients’ annual relapse rate. Another was to see if it improved a measure of brain abnormality known as magnetization transfer ratio in areas with new lesions. A decline in the ratio is associated with loss of the protective myelin coating around nerve cells and loss of nerve cell fibers called axons.
Initially researchers discovered that NGbAC1 failed to reduce inflammation between weeks 12 and 24. This prompted the team “to embark on a post hoc exploratory analysis,” Hartung said.
The new analysis showed that a “potential benefit” appeared at week 24, he said. The results suggested that the highest dose of NGbAC1 promoted remyelination in a component of patients’ brains known as normal-appearing white matter.
Almost all participants completed the study, with no safety problems or patients having difficulty tolerating the treatment during the 24 weeks, Hartung said.
The CHANGE-MS trial is continuing. The team hopes that findings on “inflammation, remyelination, biomarkers and clinical measures” at week 48 be available in the beginning of 2018, Hartung said.