Blood Levels of IgG3 Antibodies May Predict Faster Shift to MS in Clinically Isolated Syndrome Patients, Study Says
Higher-than-usual levels of specific antibodies in the blood of patients with clinically isolated syndrome (CIS) may predict a faster progression to multiple sclerosis (MS), an Australian study reports. The specific antibody is known as IgG3, an immunoglobulin known to promote inflammation.
The study, “Higher Serum Immunoglobulin G3 Levels May Predict the Development of Multiple Sclerosis in Individuals With Clinically Isolated Syndrome,” was published in the journal Frontiers in Immunology.
CIS is a first episode — one lasting at least 24 hours but typically followed by full recovery — of neurological symptoms caused by inflammation and the loss of myelin, the protective layer of nerve fibers. CIS is known to often precede the development of MS, a progressive disease marked by the immune system attacking myelin in the central nervous system (the brain and spinal cord).
Diagnosing this condition currently includes imaging scans (MRIs) to check for evidence of CNS inflammation and demyelination (lesions), and blood tests to rule out other possible causes of the symptoms experienced, which can range from vision problems (optic neuritis), to muscular weakness or extreme nausea.
No reliable biomarkers exist to that might guide prognosis, or likely outcomes, in a person with CIS, the study noted, only historical knowledge that an earlier age at CIS onset and evidence of multiple lesions (nine or more) on an MRI scan are associated with a high risk of conversion to MS.
Blood biomarkers that help to predict the likely length of time to such conversion would be of considerable value, especially in allowing for better and more timely treatment decisions.
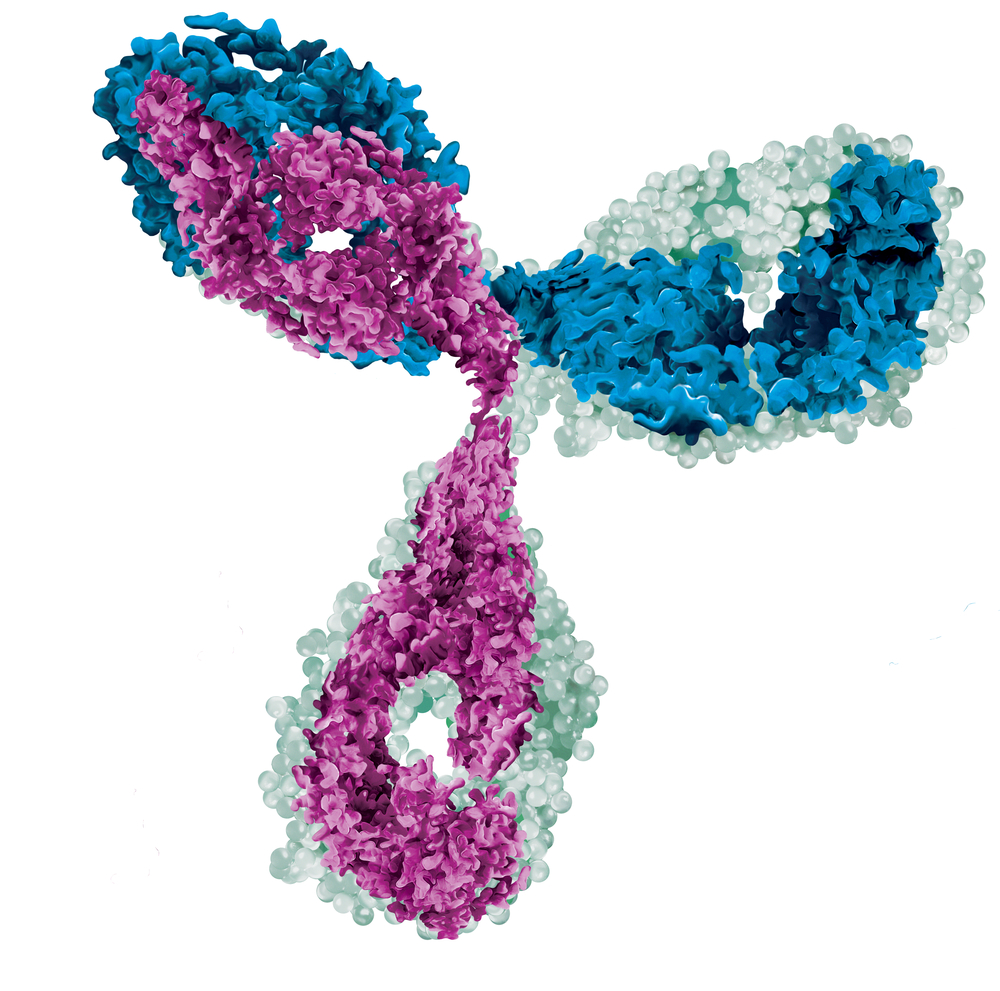
Increasing evidence has shown that B-cells — a type of white blood cell that produces antibodies against pathogens and is involved in inflammatory responses — are critical players in MS development.
Both CIS or MS patients have B-cells in the cerebrospinal fluid — the fluid that fills the brain and spinal cord – a hallmark of central nervous system inflammation and one associated with brain lesion severity. But while changes in the levels of specific antibodies have been associated with other inflammatory neurodegenerative disorders, no MS-specific antibodies have been identified so far.
Researchers in Australia investigated whether specific types of immunoglobulin (Ig) — an immune system antibody — might be specific to CIS and MS, and if so, whether they could predict rate of progression from CIS to MS.
They analyzed the levels of several Ig antibodies — IgG (IgG1, IgG2, IgG3, and IgG4 subtypes), IgA, and IgM — in blood samples of 20 people recently diagnosed with CIS, eight MS patients, and 10 healthy individuals.
Those with CIS had participated in the PhoCIS study, a trial (ACTRN 12614000185662) evaluating whether phototherapy could prevent MS conversion in a high-risk CIS group. Sixteen of these 20 patients converted to MS within 12 months of blood collection.
Results showed that CIS patients had significantly lower levels of IgG and IgG2 (which could partially explain the lower levels of total IgG) compared to healthy people.
MS patients also had significantly reduced levels and proportions of IgG2 (within IgG total levels), but increased levels of IgM and proportions of IgG1 and IgG3 compared to healthy individuals.
The team believes these differences could be markers of an MS-related abnormal production of Ig antibodies by B-cells. Researchers also found a significant association between the proportions of IgG3 and the frequency of immature circulating B-cells in CIS patients.
Further, higher levels of IgG3 and a higher proportion of IgG3 in the blood of people newly diagnosed with CIS were seen to be significantly associated with faster progression to MS.
This suggests that IgG3 levels and/or proportions of total IgG are potential predictive biomarkers of rapid conversion of CIS to MS, and could be used to guide treatment decisions in individuals with CSI, the researchers said.
Since IgG3 is known to be a potent pro-inflammatory antibody, it “could actively contribute to systemic pro-inflammatory immune responses in CIS and MS,” they wrote.
The team also noted that larger studies are needed to confirm these results and the predictive value of blood IgG3 levels in the progression of CIS to MS.






