Adult Oligodendrocytes May Replenish Myelin Production in MS, Study Suggests
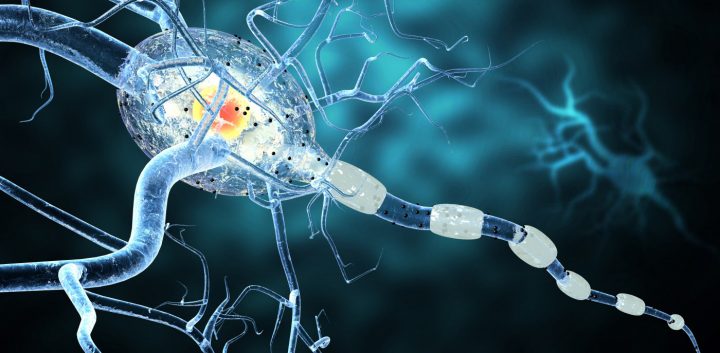
Photo by Shutterstock
Mature, adult oligodendrocytes can reacquire their ability to produce myelin to replace the ones lost in diseases like multiple sclerosis (MS) without undergoing a stem cell-like state, a new study shows.
Myelin is the fat-rich substance that wraps around nerve fiber projections (axons) protecting them and increasing the speed of the signals relayed by nerve cells. Myelin loss is the underlying cause of MS.
The study “The adult oligodendrocyte can participate in remyelination” was published in the journal PNAS.
Oligodendrocytes are the cells producing myelin, and those responsible for myelinating the nerve cells’ axons. A single oligodendrocyte is capable of myelinating multiple axons.
Mature, myelin-producing oligodendrocytes develop from more immature, stem cell-like cells, called oligodendrocyte progenitor cells. So, when myelin is lost, the only way to recover it is to have a new oligodendrocyte from progenitor cells to produce it again.
Join the MS forums: an online community especially for patients with MS.
This has been the dogma in MS research, and the reason why MS treatments aimed at remyelination have been focused on recruiting oligodendrocyte progenitor cells to the sites of myelin damage, in order to induce new myelin production.
Now, researchers at the University of Wisconsin–Madison’s School of Veterinary Medicine show evidence that mature oligodendrocytes can reactivate and produce myelin again.
Using cats and Old World monkeys, called rhesus macaques, that suffered a severe loss of myelin in their axons, the researchers showed that mature oligodendrocytes could begin re-myelinating the damaged axons.
For this to happen, researchers noticed, mature oligodendrocytes need to have connections with myelin segments — called internodes — of healthy axons.
“If this cell is still biologically active and maintaining these internodes, it can re-extend processes out to these demyelinated segments,” Ian Duncan, PhD, the study’s first author and a neuroscientist at the University of Wisconsin–Madison’s School of Veterinary Medicine, said in a press release.
“Those processes can make new myelin sheaths, which end up being thinner and shorter than the previous internodes,” Duncan added.
Researchers used a cat model of severe myelin loss in the central nervous system. In 2009, they showed that cats fed with irradiated food developed widespread and severe myelin loss. Returning these animals to a regular diet induced myelin repair and nerve cells’ function.
This new model allowed researchers to study the role of oligodendrocytes, which in other animal models, such as the mouse, are killed when using a toxin, called cuprizone, to induce loss of myelin.
“The de facto model to study demyelination and remyelination is in a mouse fed a toxin called cuprizone,” Duncan said. “But the toxin kills oligodendrocytes. So, studying the mouse, you naturally wouldn’t see any of the original oligodendrocytes beginning remyelination.”
Researchers looked at myelin sheaths in the cat’s nervous system after feeding them with the irradiated food and then back into a regular diet, and found that myelin was arranged as a mosaic; some axons had a thick layer of myelin, while in others the myelin sheaths were very thin.
The thick myelin layers are formed during embryonic development, suggesting that the thin layer of myelin must have come from surviving oligodendrocytes after an event of myelin loss.
“The most likely explanation of that mosaic appearance is surviving oligos,” Duncan said. “Thick myelin sheaths are never seen following remyelination, just thin sheaths. And surviving adult oligodendrocytes are adjacent to these sites of demyelination, making them likely candidates for myelin repair.”
The same was found when they analyzed samples of nervous tissue from a rhesus macaques model of another demyelinating disease, called sub-acute combined degeneration. The samples were stored by neuropathologist Dimitri Agamanolis, at Case Western Reserve University in the 1970s, and he shared the material with Duncan’s team.
“You see in the monkeys, too, single oligodendrocytes connected to mature myelin sheaths that also have processes extended out to and surrounding demyelinated axons,” Duncan said.
With the help of Grahame Kidd and a private research lab Renovo Neural in Cleveland, researchers were able to reconstruct 3D images of the cat nerve cells that show oligodendrocytes spreading in the spinal cord and “touching” both mature myelin and remyelinating damaged myelin sheaths.
These findings suggest that mature oligodendrocytes can indeed reactivate their myelin-producing capacity.
According to the team, in MS patients, this process may be slower, lagging behind and not able to mitigate the progression of myelin loss; alternatively, many oligodendrocytes may have lost their connection to internodes, rendering the cells inactive.
Overall, the new findings “indicate that mature oligodendrocytes can participate in remyelination,” the researchers wrote, and open new avenues for MS treatment that may help slow or even halt disease progression.






