#ACTRIMS2019 – RRMS Conversion to SPMS Is Preceded by Spinal Cord Atrophy
Written by |
The rate of spinal cord tissue loss is a strong indicator of conversion from relapsing-remitting multiple sclerosis (RRMS) to secondary progressive MS (SPMS), according to a finding presented at the fourth annual Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum 2019.
The forum is taking place in Dallas, Texas, (Feb. 28–March 2), and the results were presented by Antje Bischof, MD, from the University of California, San Francisco (UCSF).
The presentation was titled “Accelerated Cord Atrophy Precedes Conversion to Secondary Progressive Disease in Relapsing Multiple Sclerosis.”
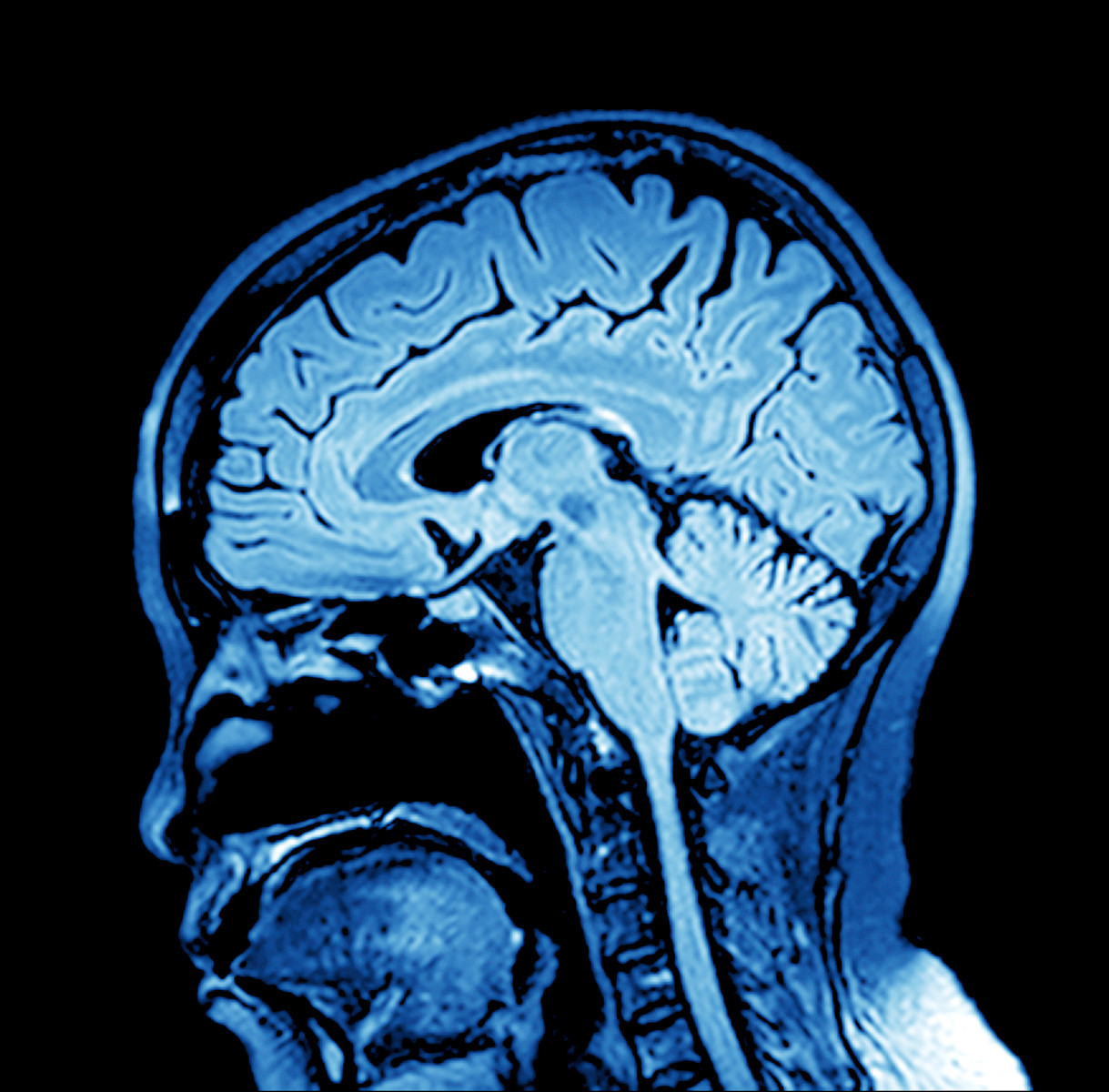
Magnetic resonance imaging (MRI) has been a useful tool to assess potential markers of disease progression and disability. MRI studies in MS patients show that a decreased spinal cord area is strongly associated with increased disability, and suggest that the spinal cord area can distinguish relapsing from progressive forms of MS.
However, the use of spinal cord atrophy (shrinkage) as a biomarker for MS disease disability and type needs to be studied further.
To address this gap, researchers at UCSF conducted a longitudinal study — meaning a study involving repeated examination of the same measures, in the same people, over a certain period of time. The study, started in 2004, evaluated spinal cord atrophy in MS patients through MRI scans over the course of 12 years.
In total, 54 RRMS patients who converted to SPMS during the 12-year observation period were analyzed. These patients were matched, based on demographic and clinical criteria, to 54 other RRMS patients who did not convert to SPMS during the same time period. In addition, 54 age- and sex-matched healthy individuals (the control group) were evaluated.
Based on brain MRIs, which included the upper spinal cord part called the C1 level, researchers analyzed brain volume and spinal cord area at C1 level to determine whether changes in these parameters could distinguish between RRMS patients who did and those who did not convert to SPMS during the observation period.
Results showed that patients who converted to SPMS had accelerated rates of spinal cord atrophy before conversion to a progressive disease course (atrophy average of 2.15% per year), compared to their RRMS matches who did not convert to SPMS (atrophy average of 0.74% per year).
Importantly, Bischof noted that this difference in rate of spinal cord atrophy could be detected up to four years before conversion to SPMS.
In contrast, measures of brain atrophy or white matter lesions — including lesion volume, and regional and global brain volumes at baseline and over time — did not discriminate between the two groups.
Furthermore, according to Bischof, relapse rate, disease duration, the presence of new or enlarging lesions, and the use of disease-modifying therapies also did not discriminate RRMS patients who converted to SPMS from those who did not convert.
Based on the results, Bischof concluded that “cervical cord atrophy (C1 level), as obtained from routine brain MRI, is a strong indicator of impending conversion to SPMS.”
The researchers suggested that “cervical atrophy rate at C1 level could be used as a prognostic marker to study the role of genetic, environmental, and immune variables on MS, and to measure the long-term impact of treatment in clinical trials.”
In addition, Bischof suggested that C1 atrophy also could be used in “early stratification [classification] of patients at risk for severe disability to guide individualized treatment decisions.”
Overall, according to the team, the annual rate of cervical cord tissue loss is “the strongest indicator among currently available imaging markers” of conversion from RRMS to SPMS.


