#ACTRIMS2019 – Evobrutinib Significantly Reduces Brain Lesions in Relapsing MS, Phase 2 Trial Shows
Evobrutinib, Merck KGaA’s oral candidate for relapsing multiple sclerosis (MS), is safe and can significantly reduce active brain lesions over 24 weeks of treatment, results of ongoing Phase 2 study show.
Xavier Montalban, PhD, MD, with Vall d’Hebron University Hospital in Barcelona, presented the results in the talk “Primary Analysis of a Randomized, Placebo-Controlled, Phase II study of the Bruton’s Tyrosine Kinase Inhibitor Evobrutinib (M2951) in Patients with Relapsing Multiple Sclerosis,” at the 4th Annual Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum, that ran from Feb. 28 to March 2, 2019, in Dallas, Texas.
Evobrutinib (M2951), developed by Merck KGaA (known as EMD Serono in the U.S. and Canada) is a highly specific, oral inhibitor of Bruton’s tyrosine kinase (BTK), which is vital for the development and functioning of several immune cells. These include antibody-producing B-cells and macrophages.
By inhibiting BTK, evobrutinib suppresses autoantibody-producing cells, a common feature in autoimmune diseases like MS.
According to Montalban, preclinical studies in animal models of MS suggested that evobrutinib could reduce inflammation in the central nervous system, and ameliorate disease severity.
The ongoing Phase 2b trial (NCT02975349), sponsored by the EMD Serono Research & Development Institute, has enrolled 267 patients, ages 18 to 65, with active relapsing MS — either relapsing-remitting MS (RRMS) or secondary progressive MS (SPMS) with relapses. The aim is to assess the safety and efficacy of evobrutinib compared to a placebo.
Participants were randomized to receive either evobrutinib, placebo, or Tecfidera (dimethyl fumarate, marketed by Biogen), a disease-modifying therapy approved for RRMS.
Those in the evobrutinib group are receiving one of three doses — low (25 mg once daily), middle (75 mg once daily), or high (75 mg twice a day) — for 48 weeks (11 months). Patients in the placebo group receive a placebo for 24 weeks, followed by low-dose evobrutinib for another 24 weeks.
Those in the Tecfidera group were given a 120 mg capsule twice a day for seven days, followed by a 240 mg capsule twice daily for 47 weeks.
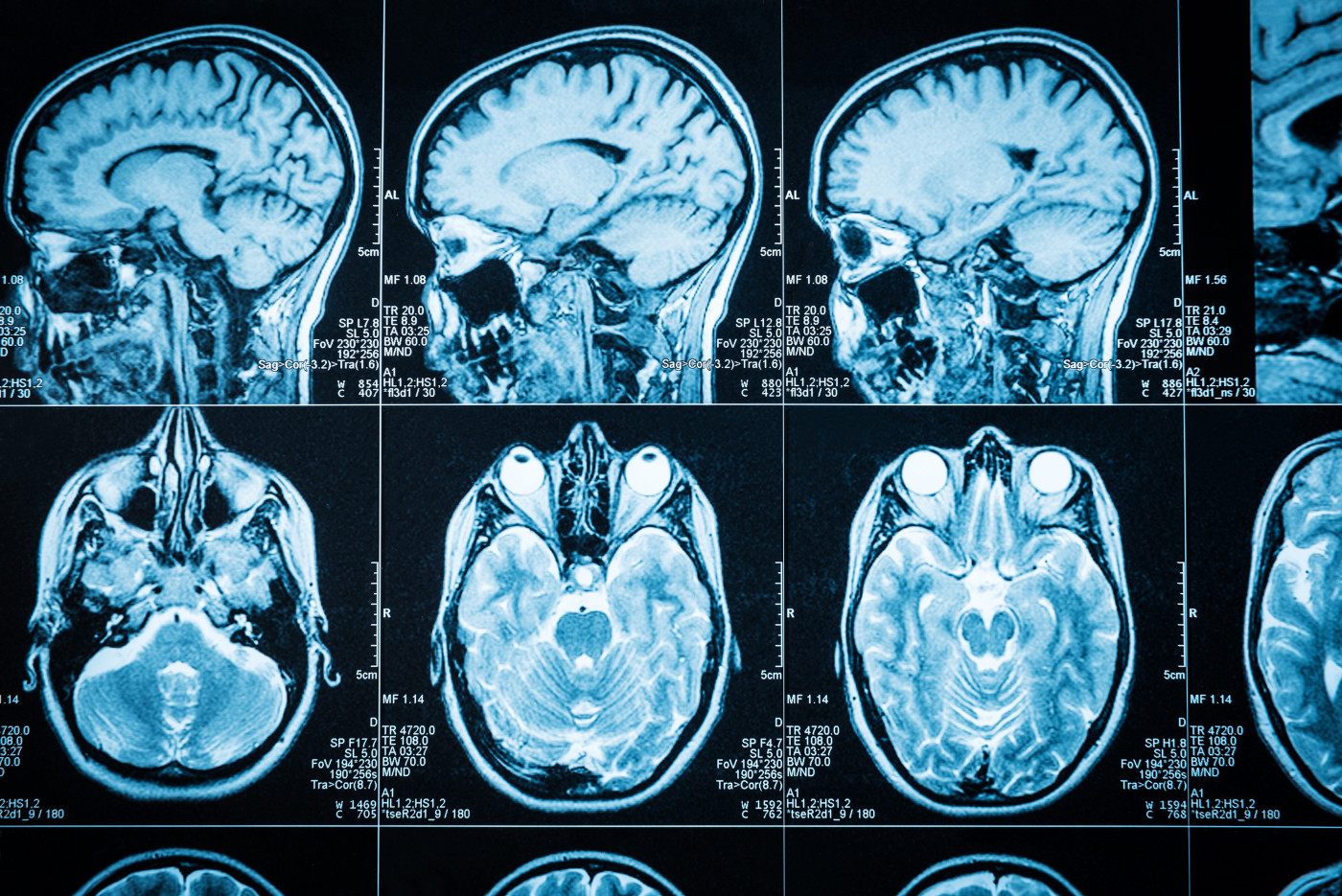
The study’s main goal (primary endpoint) is the number of active brain lesions in the three groups at different stages of the treatment — weeks 12, 16, 20, and 24. Secondary endpoints are assessments of annualized relapse rates, and the therapy’s safety profile.
Nearly all patients enrolled (244 of 267) completed 24 weeks of treatment.
Results showed that the mean number of active brain lesions (referred to as T1 lesions on MRI) measured from week 12 to 24 in patients taking evobrutinib dropped as the dose increased – 4.06 (low dose), 1.69 (mid dose), and 1.15 (high dose) — compared to those on placebo (mean number, 3.85). (The mean number seen in the Tecfidera group was of 4.78, but a treatment comparison is not the trial’s objective.)
Evobrutinib at 75 mg, either given daily or twice a day (total 150 mg), significantly reduced the number of active lesions relative to the placebo group. The low, 25 mg daily dose failed to show any therapeutic benefit.
Researchers also saw a significant trend for a reduced annualized relapse rate (mean relapse rate per year) with evobrutinib at 75 mg taken once or twice a day, with a better response at the higher dose — 0.13 in the 75 mg once daily group, 0.08 with 75 mg twice a day, and 0.37 in the placebo group. (The Tecfidera group had an annualized relapse rate of 0.20).
Treatment-related adverse events were similar between the low- and mid-dose evobrutinib groups and placebo, but higher for evobrutinib 75 mg given twice a day.
The most common was an increase in the levels of liver enzymes, indicating possible injury to the liver. All adverse events were reversible and asymptomatic, the team reported.
Evobrutinib was seen to be well-tolerated, without any cases of serious infections.
Overall, the findings support the BTK inhibitors as a potential oral disease-modifying treatment for relapsing MS.
“The observed benefit-risk profile of evobrutinib supports further clinical development,” Montalban said.
“We are proud to participate in the important scientific exchange at ACTRIMS as it aligns with our commitment to advancing MS science to address patient needs,” John Walsh, MD, vice president, neurology and immunology, U.S. medical affairs at EMD Serono, said in a press release.






