Menstruation Onset, Pregnancies and Breastfeeding Habits Don’t Influence MS Risk, Study Suggests
Written by |

A woman’s age at her first menstruation, or becoming pregnant and breastfeeding does not substantially influence the long-term risk of multiple sclerosis (MS) or the risk of increased disability, a study of a large number of patients with clinically isolated syndrome (CIS) shows.
Rather, careful clinical exams of women making “reproductive decisions” — like looking for evidence of a second relapse or brain lesions on MRI (magnetic resonance imaging) scans — and starting appropriate MS treatment early in the disease course was the study’s “main message,” the researchers concluded, providing “useful information for women with MS regarding reproductive counseling
The observational study “Menarche, pregnancies, and breastfeeding do not modify long-term prognosis in multiple sclerosis” was published in the journal Neurology.
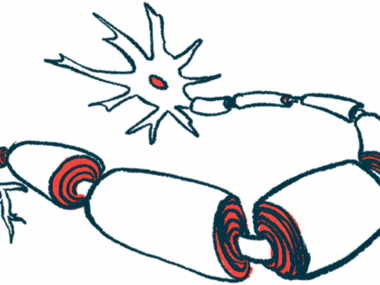
It is well-established that women are at higher risk of MS, developing the disease two to three times more frequently than men. This fact suggests gender differences in the immune system or the central nervous system, possibly caused by differences in genes, sex hormones, and/or exposure to environmental risk factors like smoking habits, and weight (high body mass index).
Yet, the role of sex-related factors in MS prognosis is still under debate.
For example, it has been proposed that an early menarche (a first menstruation, first monthly period cycle) or earlier sexual maturation amount to a longer exposure to sex hormones, which might be associated with an increased disease risk.
Other studies demonstrated that the probability of an MS attack (relapse) lessens during pregnancy, but rises shortly after the baby’s birth due to hormonal changes. But the long-term effects of pregnancy and breastfeeding on MS risk are not established.
Mar Tintoré, a neurologist and chief clinician at the Multiple Sclerosis Centre of Catalonia in Spain, and colleagues conducted a study to better understand the role of hormonal factors in modifying MS disease course. Specifically, they investigated if a person’s age at first menstruation, being pregnant before and after CIS onset, and breastfeeding played a role in her MS prognosis.
The study included 501 female participants, all under age 50, recruited from a group of CIS patients who had been followed since 1995. As these people were evaluated clinically on a regular basis, their data were used to determine the risk of MS and of becoming disabled.
Three outcome measures were used to evaluate the risk: developing clinically defined MS, having a MS diagnosis according to the McDonald 2010 guidelines, and reaching a Expanded Disability Status Scale (EDSS) score of 3.0, corresponding to a mild disability level. Additionally, the prevalence of second attacks (relapses) was also analysed.
Patients also completed a survey that collected information about their age at first menstruation, number of pregnancies, exposure to hormones (hormonal contraceptives, fertility treatment, hormone replacement therapy), and other environmental risk factors (smoking, body composition at menarche, and vitamin D levels).
During the follow-up period, 53% of these patients had a second relapse, and 61% met the McDonald 2010 MRI MS criteria. Regarding disability, 13.4% reached a confirmed EDSS score of 3, and 2.6% an EDSS score of 6 (the higher the score, the worse is the patient’s disability).
Results demonstrated that women’s age at first menstruation did not correlate with the age at CIS onset, nor with the risk of a MS diagnosis, a worse disability or a second attack.
Pregnancy before or after CIS onset also did not seem to affect significantly a women’s likelihood of developing MS or of becoming more disabled. The same was true with breastfeeding.
The team concluded that “the prognosis of MS will not be significantly affected by pregnancy once all other variables are considered,” they wrote.
“In this regard, the clinical activity, MRI findings, and early initiation of treatment are the most important prognostic factors that should be considered when addressing reproductive decisions,” they added.
Hormones might play an important role in the risk of the disease, the researchers noted, but this effect may diminish once the disease is established.
They noted that further studies are needed to better understand the impact of a women’s reproductive history over MS disease course.