Clinical Benefit of Relapsing-Remitting Multiple Sclerosis Therapies Highlighted in Review
Written by |
A review study recently published in the journal Cochrane Database of Systematic Review (CDSR) focused on the clinical benefit of different therapies available for relapsing-remitting multiple sclerosis (RRMS). The study is entitled “Immunomodulators and immunosuppressants for relapsing-remitting multiple sclerosis: a network meta-analysis” and was led by researchers at Fondazione I.R.C.C.S. Istituto Neurologico Carlo Besta in Italy.
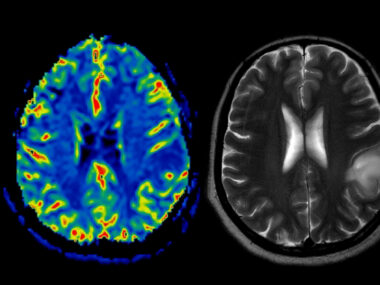
MS is a chronic, progressive neurodegenerative disorder that results from an attack on the central nervous system (brain, spinal cord and optical nerves) by the body’s own immune system, resulting in motor function impairment, irreversible neurological disability and paralysis. The most frequent form of the disease is RRMS, which is clinically characterized by recurring episodes of neurological symptoms. It is estimated that more than 2.3 million people in the world suffer from MS and there is currently no cure.
Several therapeutic approaches are currently available for RRMS treatment including immunosuppressants, immunomodulators and biologics. These therapies have been shown to reduce the frequency of disease relapse in patients; however, their potential effect in delaying new relapses or the worsening of the disability characteristic of MS is not clear.
In the study, researchers compared the clinical benefits and acceptability of specific RRMS therapies, namely interferon beta-1a (Avonex, Rebif), pegylated interferon beta-1a, interferon beta-1b, glatiramer acetate, fingolimod, natalizumab, dimethyl fumarate, mitoxantrone, daclizumab, alemtuzumab, laquinimod, azathioprine, teriflunomide, and immunoglobulins. The team also investigated the proportion of patients who withdrew from treatment due to adverse events.
The team analyzed data from randomized controlled clinical trials that focused on one or more of the RRMS therapies mentioned above, comparing them to a placebo or other active agent in adult patients with RRMS. In total, 39 studies involving 25,113 participants were included in the review. The median duration of the trials included was 24 months, and 60% of them were placebo-controlled trials while 40% were head-to-head studies.
Researchers found that fingolimod, natalizumab, mitoxantrone and alemtuzumab outperformed other drugs in terms of providing a protective effect against relapse recurrence in RRMS patients during the first 24 months of treatment. The most effective drug among those analyzed was found to be alemtuzumab, followed by mitoxantrone, natalizumab, and fingolimod. In terms of disability worsening, the drugs with the most protective action were mitoxantrone, alemtuzumab, and natalizumab. In terms of treatment withdrawal, almost all the drugs analyzed in the review were linked to adverse events and subsequently a higher proportion of participants who withdrew in comparison to placebo treatment.
RELATED: New Multiple Sclerosis Drug May Repair Nerve Demyelination
The research team concluded that overall, alemtuzumab, natalizumab, and fingolimod are the best treatment choices for averting clinical relapses in RRMS patients, although this conclusion is limited to the first 24 months after therapy. In terms of preventing disability worsening within the 24 months period analyzed, only natalizumab offered a significant beneficial effect; although authors emphasize that there is insufficient evidence available to evaluate the prevention of irreversible disability worsening for all treatments considered.
The authors highlight that the clinical benefit of all the therapies investigated beyond two years is uncertain; this is a relevant fact since MS can last 30 to 40 years. Since most of the data available for these therapies were collected from short-term trials, data on drug safety profiles is limited to a short time-frame. The team also emphasizes that more than 70% of the studies analyzed were sponsored by pharmaceutical companies, a fact that may have influenced some of the results reported. The team suggests that in the future, randomized trials based on direct comparison between the different treatment options should be conducted, that trial cohorts should be followed-up for longer periods, and that more research is required to establish the medium and long-term clinical benefit and safety of the different agents.