Expert Voices: Understanding and managing fatigue in multiple sclerosis
Written by |

In this installment of our “Expert Voices” series, Multiple Sclerosis News Today asked Meghan Beier, PhD, a rehabilitation neuropsychologist who teaches skills and techniques to improve patients’ quality of life, to answer some of your questions related to fatigue for people with multiple sclerosis (MS).
Beier is a psychologist specializing in MS at the Johns Hopkins University School of Medicine. She founded FindEmpathy.com, an online directory that helps patients with medical conditions find specialized mental health providers. She has served as a consultant and speaker for organizations such as Can Do MS, the National MS Society, the MS Association of America, MS Hope Day, the American Academy of Neurology, and the MS Coalition. Additionally, she has been featured in publications such as People Magazine, Momentum Magazine, Everyday Health, and Psychology Today. In 2018, Beier was part of an expert panel that established national guidelines for assessing and treating cognition in people living with MS.
What typically causes fatigue for people with MS?
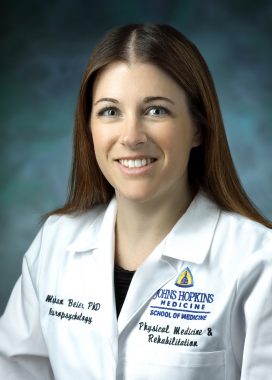
Meghan Beier is a rehabilitation neuropsychologist and an active researcher interested in cognitive rehabilitation and healthy aging for individuals with MS. (Photo courtesy of Meghan Beier)
The neurologic cause of fatigue is still under investigation. However, fatigue in people with MS can be triggered by many things, such as heat sensitivity, infections like a urinary tract infection or the common cold, cognitive or physical overexertion, and exacerbations. This is not an exhaustive list.
Additionally, co-occurring medical conditions can add to or worsen fatigue. For example, many people with MS have sleep disorders or sleep apnea. If sleep is impacted, it is going to be harder to recover your energy. Depression can also make fatigue worse, and we know approximately 50% of people with MS will experience depression at some point in their life.
Fatigue is a real and impactful symptom that many people who do not have MS struggle to truly understand.
What characteristics differentiate MS fatigue from the exhaustion a healthy individual might experience?
The fatigue experienced by people with MS is very different than the exhaustion that a healthy individual might experience. It can be triggered by activity, but it can also just be present for no apparent reason. When fatigue is bad, it can be so impactful that it causes someone not to be able to move, or struggle to do simple tasks like pick up a coffee cup. Additionally, it’s one of the primary reasons that people with MS end up leaving their job. It’s not just “feeling tired.”
Any suggestions for how to navigate explaining these differences to a loved one who doesn’t understand MS fatigue?
I often recommend using metaphors. One I like to use is the illustration of energy being like the battery on your cellphone, especially the older versions that didn’t have the battery lengths we are seeing today! Without plugging it in regularly throughout the day, it will stop working and will take hours to recharge. Once it is out of battery, it can’t function. However, I find that people with MS have lots of creative ways of explaining their fatigue, so if you can’t think of a good way, Google illustrations or ask someone in your support group.
If loved ones still don’t get it, take them to a doctor’s visit or an educational event, like those hosted by Can Do MS. Sometimes hearing about fatigue from a medical provider or expert organizations can help loved ones realize this is a true symptom with a real impact.
At what point would fatigue be considered medically worrisome for a person with MS?
If fatigue impacts the things you want to do or need to do — your hobbies, enjoyed activities, your work, or your relationships — then it should be addressed. Anything impacting your everyday functioning is worth discussing with your medical team.
Does cognitive decline affect energy levels? If so, how?
Anecdotally, many of my patients notice a link between cognition and fatigue. And it makes sense. Many of our daily activities function on autopilot.
For example, many of us don’t have to think about what order we put on clothes or how to make a cup of tea. We just do it. This helps to save energy for our brains and bodies. But with MS, these activities become much more conscious. If you have balance problems, while walking, you may have to consciously notice where your foot is in space and whether it is landing on the ground correctly. You may have to consciously think about moving your fingers in a way that allows you to button a shirt. Or if you are in the shower and the water is warm, you may have to consciously think about staying stable while closing your eyes so you don’t lose your balance.
That conscious effort takes energy and can be fatiguing. When cognition is impacted by MS, it also becomes less automatic. It takes longer to write an email or organize your thoughts. You must consciously think about a recipe and whether you use one or two cups of flour. It becomes a more conscious and less automatic process, thereby more fatiguing.
Can a patient treated for MS-related depression expect a noticeable boost in energy?
It is possible that treating depression can boost energy, but it may not fully remove fatigue. As described earlier, fatigue is a symptom of MS itself, and depression may worsen the experience. I will always advocate for adequately treating depression, and it can have a noticeable impact on fatigue, but may not take away the symptoms entirely.
Is there anything people with MS can do nutrition-wise to combat fatigue? Are there any specific diets that may be beneficial?
Based on my reading of the research, there is no one specific diet that is perfect for every person with MS. However, the underlying theme of many of the diet trials is that fatigue and mood are improved with healthier eating. This means generally eating more colorful whole foods like fruits and vegetables, and less processed food, sweets, or fried food.
A registered dietitian colleague of mine, Mona Bostick, recommends the 80/20 rule. Try to eat healthy whole foods 80% of the time and indulge 20% or less of the time. It is important to strive toward healthy eating, but avoid rigid strict rules that may impact social relationships, be overly expensive, or trigger feelings of guilt and shame if we are not eating “healthy enough.” Balance is the key.
Finally, I often hear from people with MS that cooking at home can be challenging due to MS. So trying things like batch cooking, getting your family to help, or making more simple meals can be helpful.
Why does heat so strongly affect MS fatigue? Any tips for countering this challenge?
Even a quarter to half a degree of change in body temperature can trigger a “pseudo-exacerbation.” A pseudo-exacerbation is when someone experiences MS symptoms at greater intensity, or symptoms that resurface in the face of heat, infection, or for other reasons. If fatigue is a symptom of your MS, heat may trigger this pseudo-exacerbation, temporarily worsening fatigue. Cooling techniques can be very beneficial. There are cooling vests and neck towels. I’ve also heard of people putting their feet in a cold-water bath.
Any other tips for managing MS fatigue, especially amid an acute attack?
Pacing. As with the example of the cellphone above, we have found that if people take short breaks throughout the day and use tools to conserve energy, their energy lasts longer. Don’t go, go, go until you are wiped out. Doing this often leads to more frustration and longer recovery times. Schedule dedicated time to sit, rest your eyes, and disconnect. This could be as short as a minute or up to 10–15 minutes. Do not sit and play on your phone or watch TV. Try to really let your brain and body rest. This will be a challenge for many individuals who are not used to resting. However, we often find that people accomplish more with rest because they do not need as many “recovery days.”
***
Expert Voices is a monthly series involving a Q&A with an expert in the MS space about a specific topic. These topics and questions are curated from a survey in which we ask readers what they want to learn more about from experts.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.