Guidelines Issued for Monitoring of MS Patients on Natalizumab Treatment
Written by |
A panel of neurologists from the U.K. and Ireland recently developed practical consensus guidelines for monitoring multiple sclerosis (MS) patients on natalizumab (Tysabri) therapy for the risk of developing progressive multifocal leukoencephalopathy (PML), a life-threatening viral infection caused by the John Cunningham (JC) virus.
The panel was summoned by Biogen but worked independently of the company, and members did not receive financial reimbursement for their work. They analyzed available data from clinical trials and real-life use. Their findings were published in the article“Stratification and monitoring of natalizumab associated progressive multifocal leukoencephalopathy risk: recommendations from an expert group,” which appeared in the Journal of Neurology, Neurosurgery & Psychiatry.
Natalizumab, used for the treatment of highly active relapsing-remitting MS (RRMS) in patients, has been associated with the development of PML. Before the age of immunomodulating biological drugs, PML was associated with immunosuppression but not with autoimmune diseases such as MS. The JC virus is common and usually benign, and infects an estimated 60 percent of the European population. But the type causing PML is a mutated form that can enter into the brain, and researchers are puzzled as to why the virus mutates in MS patients on natalizumab.
Active monitoring during treatment is necessary to reduce the risks of PML, but until now, there has been no consensus on best monitoring practices.
Known risk factors for developing PML are previous immunosuppressive therapy, as well as treatment with natalizumab for more than 25 months. A patient’s overall risk of developing PML is 1 in 1,667 during treatment of up to two years (24 months), and that risk increases to 1 in 192 patients for treatment durations of 25–48 months.
Also, the presence of antibodies against the virus before symptoms occur has been detected in the majority of patients developing PML. The Committee for Medicinal Products for Human Use currently recommends anti-JCV antibody testing every six months to identify early patients whose antibody status has changed from negative to positive. The levels of antibodies against the virus — known as the anti-JCV antibody index — has also been associated with the development of PML in patients without previous immunosuppressant therapy. This test is sensitive in predicting PML infection, but the specificity is low since many patients with high antibody levels never develop PML.
The consensus group suggested that patients should be stratified into two risk groups based on their antibody levels and other risk factors: low-risk patients in the group having an anti-JCV index equal or less than 1.5, and high-risk patients with an index above 1.5. Patients in the low-risk group are recommended to repeat antibody testing at six-month intervals, as only 1 in 5,882 MS patients with an index of 1.5 or lower and natalizumab treatment of less than two years has developed PML.
This risk subsequently increases with both treatment time and antibody levels, and an index value of 0.9 or less carries a risk of 1 in 1,961, rising to 1 in 885 if index values increase to 1.5 during years two to four of natalizumab treatment. Longer exposure further increases the risk somewhat, to 1 in 1,724 for index 0.9 or lower, and to 1 in 730 for index 1.5 during months 49-72.
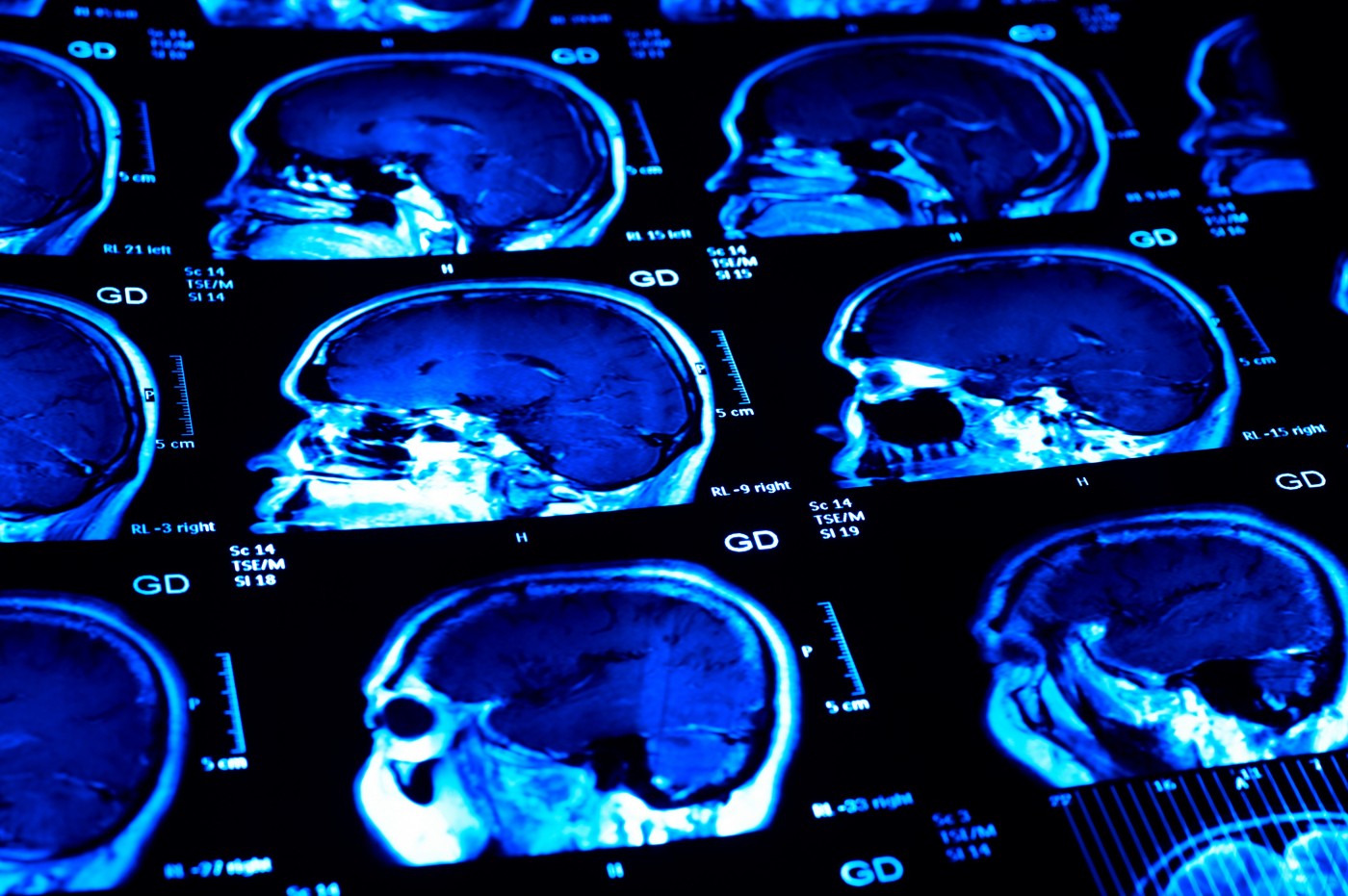
Studies have suggested that MRI detection of presymptomatic PML might improve outcomes by reducing morbidity — including permanent brain damage — and death. Individuals with all three risk factors need to be monitored closely. The consensus group recommended that MRI scans be used for monitoring during treatment, and again six months after discontinuation. High-risk patients are recommended to go through more frequent MRI scans. Earlier studies show that lesions indicative of PML have been detected up to six months before symptom outbreak, but negative MRI findings do not necessarily exclude the development of PML. The panel, therefore, recommended that if a clinician suspects PML in spite of the absence of MRI findings, frequent testing of the cerebrospinal fluid and continuing MRI scans should be performed.
The panel also recommended that all new patients receiving natalizumab have an MRI scan before treatment onset — as a reference scan — and then annually to increase the chance of detecting new lesions.
After 12 months, MRI frequency should be adapted to JCV index status or levels. JCV positive patients should have annual scans during up to 18 months of treatment. After that, MRI frequency should be increased to at least one every six months for low-risk patients and to one every three to four months for high-risk patients.
The group also pointed out that any new lesions detected on MRI, suspected to be due to PML, should lead to treatment discontinuation until PML has been, as far as is possible, ruled out.
Since it is not known how the anti-JCV index changes over time, the panel suggested that their recommendations might need updating as new evidence emerges. Since data was not available to support some of the guidance, the group based its recommendations on members’ clinical experience.
High-risk does not infer a contraindication for the drug’s use, members said. “Given the clinical impact of natalizumab, a positive test for anti-JCV antibodies is not a contraindication for natalizumab treatment; neither is an anti-JCV antibody index >1.5 a contraindication to continue natalizumab treatment,” the panel concluded in its report.


