Inflammation Fighters in Blood Cells Seen to Attack in Entirely New Way
Written by |
To reach tissues infected with foreign agents, neutrophils, the body’s first line of defense, need to travel through vessel walls — and do so by switching on a class of adhesion receptors, called integrins, that bind to other adhesion molecules at the surface of the capillary walls. Now, in a recent paper published in Nature Communications, researchers revealed an entirely new way through which neutrophils activate their integrins in preparation to cross a vessel wall.
The study, “Neutrophil recruitment limited by high-affinity bent β2 integrin binding ligand in cis,” was developed by researchers at La Jolla Institute (LJI) for Allergy and Immunology, and may lead to the development of new and targeted strategies that either dampen immune responses, as is required in diseases like multiple sclerosis that are associated with chronic inflammation, or boost them in response to foreign pathogens.
“Once neutrophils sense a site of infection behind a capillary wall, they need to get out of circulation fast. Previously, we knew they initiated that by switching on adhesion molecules to grab onto a vessel in less than a second,” Klaus Ley, MD, who led the study and is a professor and head of LJI’s Division of Inflammation Biology, said in a press release. “In our new study we have discovered an unexpected way that these molecules change their shape to do that.”
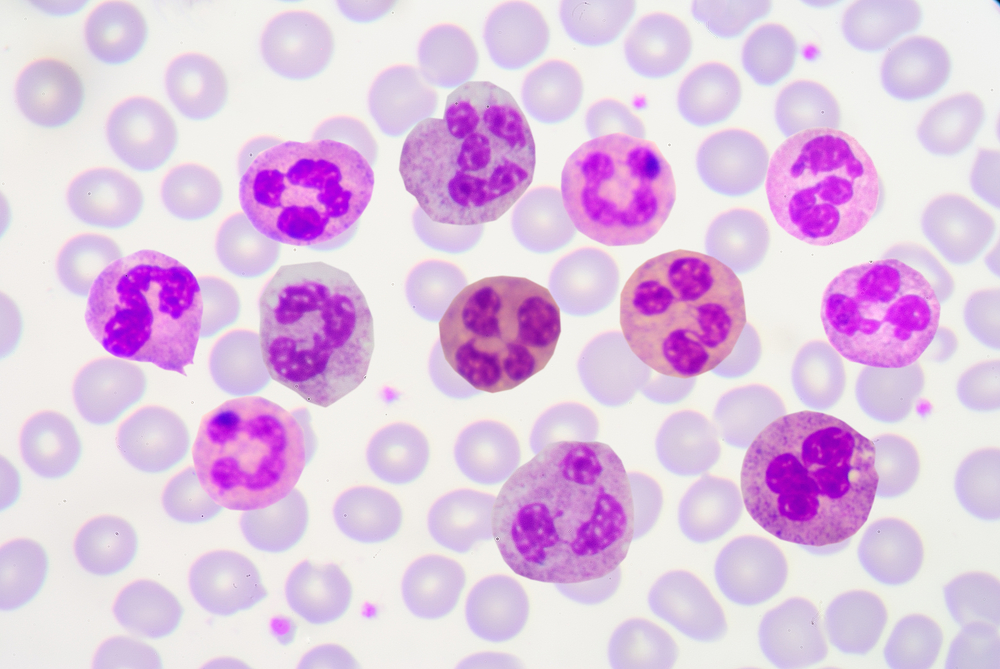
Neutrophils, the most abundant type of white blood cells, work to form the first line of defense against pathogens by recognizing, trapping, and eliminating bacteria, virus, and other infectious agents. They spend their lives traveling across the bloodstream looking for such agents, but do most of that work outside the blood vessels.
When neutrophils reach infected sites, they halt on a dime and cross the vessel wall through the activation of particular integrin molecules. Until now, researchers thought that integrin receptors became active through a “switchblade” mechanism. The resting integrins, which are bent and minimally adhesive in neutrophils that are traveling the bloodstream, go through two sequential changes when neutrophils reached a site of infection: First, the receptor acquires a straight position, and, second, its adhesive part opens. These changes expose the hidden adhesive part of the integrin receptor that then binds to ICAM-1, the integrin present in blood vessel cells.
Although researchers found that mechanism is true in some neutrophil clusters, in other clusters, they saw that integrins assumed an unorthodox and unexpected shape, one in which the adhesive part of the receptor was already opened, but the receptor remained in a bent conformation — as if step two had occurred before step one.
Interestingly, the researchers found that even though the adhesive part was already exposed, it was bound to ICAM-1 molecules found at the surface of that same neutrophil, impairing it from binding the ICAM-1 molecules at vessel walls.
“In the old view, as neutrophils rolled along, the receptor would remain coiled like a rattlesnake with its head tucked in until it encountered its ligand. Then the head would pop up with its jaw wide open, ready to bite,” Ley said. “Our findings suggest that the snake’s mouth can be open even when its neck is down, as if it is biting its own tail.”
This discovery may be quite important to inflammation-related diseases. Researchers have already developed monoclonal antibodies able to block the interactions between neutrophil integrins and proteins at the vessel wall, and they are approved treatments for multiple sclerosis, coronary artery disease, and inflammatory bowel disease.
“This inhibitory mechanism opens the door to a new class of integrin modulators that work by a totally different principle,” Ley said. “Now, rather than designing new drugs to block the high affinity site, we could create small molecule drugs to counter inflammation by keeping the receptor in the auto-inhibited mode.”
Researchers believe such the new drugs may be less expensive and easier to administer, as they will not need to be infused as are monoclonal antibodies. In addition, other molecules could be designed to do the exact opposite, forcing the receptor to acquire an active conformation, which may improve immune responses in infection settings.


