Women with MS Have Higher Prevalence of Sexual Dysfunction, Study Reveals
Written by |

Women with multiple sclerosis (MS) are more likely to experience sexual dysfunction and sexual distress than those without the disease, a study reports.
According to researchers, the high prevalence of sexual problems among these women may be linked to their age, degree of physical disability, and depression.
The findings of the study, “Prevalence and Psychopathological Determinants of Sexual Dysfunction and Related Distress in Women With and Without Multiple Sclerosis,” were published in The Journal of Sexual Medicine.
Sexual dysfunction is estimated to affect from 40–83% of women with MS, “with the most common complaints being reduced libido, difficulties in achieving orgasm, decreased vaginal lubrication, decreased vaginal sensation, and dyspareunia [painful sexual intercourse],” the researchers wrote.
Although specific causes of sexual dysfunction in female MS patients is still being debated, a previous study considered them to be:
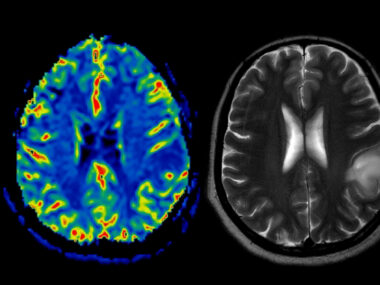
- primary, when it stems directly from the neurological damage caused by MS, leading to reduced sexual desire, vaginal lubrication, arousal, alterations in genital sensation, and difficulties achieving orgasm;
- secondary, when it arises from physical alterations brought on by MS, such as muscle tightness (spasticity), or fatigue;
- tertiary, when it is caused by emotional and/or social problems.
Although thought to be common, the prevalence of sexual dysfunction may be underestimated among women with MS, due to inconsistent use of validated diagnostic tools.
Researchers at the University of Bologna, set out to examine the prevalence of sexual dysfunction in women with MS in Italy, compared to a similar group of healthy women, using a set of validated diagnostic tools.
The observational study involved a total of 153 MS patients (mean age, 47.3 years) and 153 women without MS (mean age, 48.5). All were asked to complete the Female Sexual Function Index (FSFI, a 19-item questionnaire) and the Female Sexual Distress Scale (FSDS, a 12-item questionnaire) to assess sexual dysfunction and sexual distress.
Demographic, gynecologic, and neurologic data were collected for study participants. Patients’ physical disability was measured using the Expanded Disability Status Scale (EDSS), and mental health was assessed using the Profile of Mood State (POMS, a 65-item questionnaire), and the Beck Depression Inventory II ( BDI-II, a 21-item questionnaire).
The percentage of women with BDI-II scores suggestive of clinical depression (scores greater than 14) also was higher in patients with sexual dysfunction than in those without sexual dysfunction (32% vs 8.7%).
Correlation analyses identified a negative correlation between FSFI global scores, women’s age, EDSS scores (degree of physical disability), and BDI-II scores (depression severity), meaning that age, disability, and depressive symptoms were associated with greater levels of sexual problems.
“Our data confirm that impairment of sexual function is more common in women with MS than in women without MS. Given the impact of SD [sexual dysfunction] on quality of life, mental health, and intimate relationships, sexual function investigation should always be a standard part of the consultation with healthcare professionals for MS,” the researchers wrote.
“Future research in this field should confirm the nature of the association between depression and SD, and evaluate the impact of each treatment on the sexual function of women with MS,” they added.