Small Changes in Genes May Affect Myelin Production, Study Suggests
Written by |
The small variants seen in the DNA code among individuals may affect the ability of oligodendrocytes to produce myelin, the protective coat surrounding neurons and whose destruction is a hallmark of multiple sclerosis (MS), a study reported.
These findings open the possibility of new therapeutic options that target the underlying cause of MS.
The study “Cell type specificity of intralocus interactions reveals oligodendrocyte intrinsic mechanisms for multiple sclerosis” was published in the journal Cell.
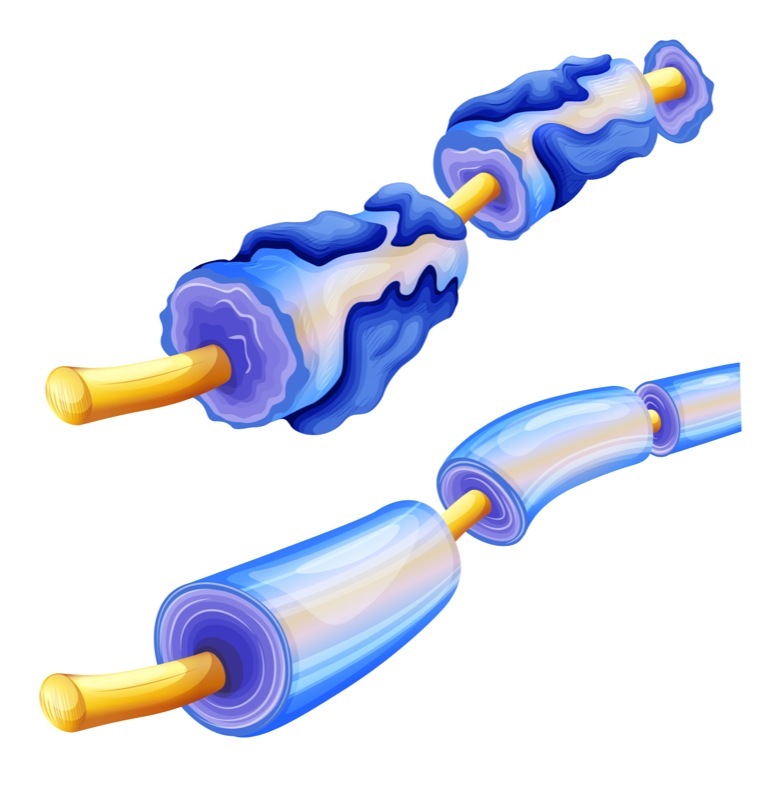
In MS, the immune system attacks myelin, the protective sheath that surrounds nerves. Myelin works as an insulator, allowing electrical signals to be efficiently transmitted; when damaged, nerves have trouble transmitting messages, leading to the disease’s hallmark symptoms.
Due to the crucial role played by immune cells, current MS treatments try to slow the disease by limiting immune reactions, and by controlling symptoms. They do not reverse myelin damage, and often fail to stop MS progression.
Due to the lack of myelin regeneration and lost of neurons, researchers suspect that the immune system is not the only player to blame.
Previous studies have shown that individuals carrying certain gene variants are at higher risk for developing MS. Exploring how these genetic changes cause disease could lead to the discovery of new therapeutic targets.
Researchers at the Whitehead Institute, in Cambridge, Massachusetts, investigated how MS-related variants affect cells from different tissues, including immune and neuronal cells.
“The idea that only genetic variants that affect your immune system are important in MS always struck me as incongruous with the way that the brain is so impacted,” Olivia Corradin, PhD, the study’s lead author, said in a Whitehead news story.
“Although the disease is primarily autoimmune, it makes sense that some aspect would be intrinsic to the brain,” she added.
Corradin’s research group used a genomic approach to identify cell types in which known variants could cause disease. Their technique is called an ‘outside variant approach,’ and takes into consideration not only variants to the DNA but also their 3D location within a cell’s nucleus.
In this way, researchers can identify DNA sequences that are far apart in the DNA sequence, but are actually neighbors when taking into account their 3D location.
Using this approach, the team selected outside variants — regulatory DNA sequences that are 3D neighbors of MS risk variants, and that targeted the same gene. If the presence of an outside variant combined with its MS risk variant increased the overall risk for MS, researchers would look for a cell type where these two variants were active.
Most of the variants were, in fact, found to be affecting both T- and B-cells, immune cells known to play a role in MS. Yet two risk variants affected oligodendrocytes. Oligodendrocytes are the myelin-producing cells found in the central nervous system (brain and spinal cord).
Next, the team studied how these two variants affected the ability of oligodendrocytes to work as intended. This was done in collaboration with Paul Tesar at the Case Western Reserve University School of Medicine.
They discovered that the process that converts the DNA code into messenger RNA (the molecules used to produce proteins) was abnormal in immature oligodendrocytes with these genetic variants. This disruption may keep oligodendrocytes from maturing, and producing myelin.
“These data implicate cell-intrinsic aberrations outside of the immune system, and suggest new avenues for therapeutic development,” the researchers wrote.
Their findings suggested that therapies promoting the growth and maturation of oligodendrocytes could help restore myelin production in MS.
Researchers hope their outside variant approach may also be used to study other complex diseases that, like MS, result from a combination of genetic and environmental factors, including cancer, and cardiovascular and psychiatric conditions.
“With complex diseases, there is a huge amount of variation among patients, in terms of both genetics and disease progression, and the same treatment is not equally effective for every patient,” said Anna Barbeau, the study’s first author.
“Our approach can lend insight into developing novel therapeutics that might benefit people who don’t respond well to existing treatments,” Barbeau added.


