Gut Bacteria Working in Concert May Promote MS, Early Study Suggests
Written by |
Two specific bacteria present together in the gut led to more immune attacks on myelin and harsher symptoms in a mouse model of multiple sclerosis (MS).
These findings add to existing evidence supporting the link between gut microbiota and MS, and highlight the need to consider potential combined effects of these microorganisms.
Future studies are needed to confirm these findings in MS patients, and possibly develop ways of treating this autoimmune disease by targeting intestinal microbiota.
The study, “Gut microorganisms act together to exacerbate inflammation in spinal cords,” was published in the journal Nature.
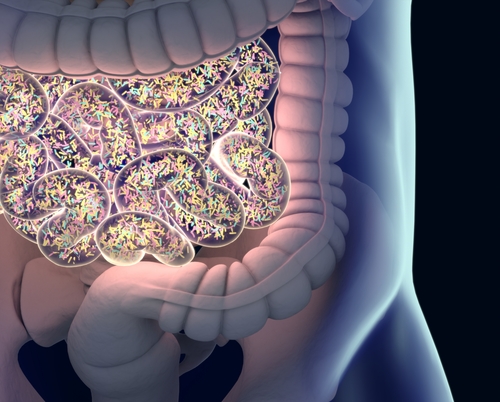
Gut microbiota — a vast community of friendly bacteria, fungi, and viruses that colonize the gastrointestinal tract — help to maintain a balanced gut function, protect against disease-causing organisms, and influence the host’s immune system and inflammatory responses.
Increasing evidence points to gut microbiota as an important contributor to MS development or severity, with MS patients showing a gut microbiota imbalance toward pro-inflammatory microorganisms.
However, how gut microorganisms promote inflammation and immune attacks against myelin — the protective sheath that covers nerve fibers and is wrongly targeted in MS — in the central nervous system (CNS; the brain and spinal cord) remains unclear.
A team of researchers at the RIKEN Center for Integrative Medical Sciences (IMS), in Japan, shed light on these mechanisms and the identity of the potential players in an experimental autoimmune encephalomyelitis (EAE) mouse model of MS.
While a particular cocktail of antibiotics was previously shown to ease MS severity in this model, the team found that ampicillin, one such antibiotic, had a similar, and significant, weakening effect.
“We found that treatment with ampicillin, and only ampicillin, selectively reduced activity of T-cells that attack an important protein called myelin oligodendrocyte glycoprotein [MOG], which helps myelin stick to neurons,” Hiroshi Ohno, MD, PhD, the study’s senior author, said in a press release.
T-cells are a type of immune cell that recognize and promote immune responses against foreign molecules. The overactivation of a particular type of pro-inflammatory T-cell, called Th17, is a main driver of inflammation and attacks against myelin in MS. MOG is also the main target of immune attacks in this mouse model of MS.
Treating these mice with ampicillin dropped T-cell numbers and MOG-induced production of pro-inflammatory molecules in the small intestine. This suggested that gut microorganisms — particularly those killed by ampicillin in this case — can activate MOG-reactive T-cells in the small intestine, which may subsequently attack myelin in the CNS.
Further experiments to identify the responsible microorganisms revealed that a new strain of the Erysipelotrichaceae family of bacteria, called OTU002, was the only microorganism almost completely eradicated from the small intestine of ampicillin-treated mice.
The researchers noted that this strain appeared to be related to bacteria previously linked to Th17 cells and found in the gut of other mammals, including humans.
To confirm that OTU002 was the culprit, the team examined germ-free EAE mice whose small intestine was colonized only with OTU002. These mice, indeed, showed more severe MS symptoms, had higher numbers of Th17 cells, and a stronger immune response to MOG than fully germ-free mice.
“But there was a problem,” Eiji Miyauchi, the study’s first author, said, noting that “symptoms in the OTU002-only mice were not as bad as those in the regular [EAE] model mice.”
This suggested that other bacterial members of the gut microbiota also contributed to MS development in these mice.
The team hypothesized that some gut bacteria could be naturally producing a molecule similar to MOG, inadvertently activating MOG-reactive T-cells. Such an event was previously reported in another autoimmune disease.
Results of shotgun genome sequencing showed that a molecule produced by the Lactobacillus reuteri bacterium mimicked a region of MOG, and when tested, it weakly activated MOG-reactive T-cells.
Notably, small intestine colonization with only L. reuteri did not worsen MS in these mice, indicating that the MOG-like molecule alone was not sufficient to affect MS severity.
However, when mice’s small intestines were simultaneously colonized with both bacteria — OTU002 and L. reuteri — MS severity greatly increased, more closely resembling what happens in the original EAE mice model.
“Here we show that two distinct signals from gut microorganisms coordinately activate autoreactive T cells in the small intestine that respond specifically to myelin oligodendrocyte glycoprotein,” the researchers wrote.
They proposed that L. reuteri’s MOG-like molecule inadvertently triggers MOG-reactive Th17 cells, while OTU002 boosts their growth and disease-associated activity.
“Our data emphasize the necessity of considering the synergistic [cumulative] effects of intestinal microbes on autoimmune diseases and give hope to people looking for effective treatments for multiple sclerosis,” Miyauchi said.
“But, because gut microbes and T-cell binding locations on myelin differ between mouse and human, further studies using human microbes and autoreactive T-cells are now needed,” Miyauchi added.
Future studies will also have to show direct evidence that these “small-intestinal MOG-reactive T cells themselves migrate into the central nervous system” to promote MS development and progression, the researchers wrote.


