Simple Sugar Molecule May Be Potential Myelin-repairing Therapy for MS

Oral administration of N-acetylglucosamine (GlcNAc) — a natural simple sugar sold as a dietary supplement — prevents myelin degeneration and loss of motor function in a mouse model of multiple sclerosis (MS).
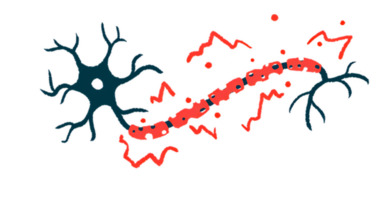
Myelin, the protective sheath around nerve fibers that helps to speed transmission of signals between nerve cells, is damaged and lost in MS.
“We found that N-acetylglucosamine activates [myelin-producing cells] to promote primary myelination and myelin repair,” Michael Demetriou, MD, PhD, the study’s senior author and professor of neurology, microbiology, and molecular genetics at University of California–Irvine (UCI)’s School of Medicine, said in a press release.
“Our data raise the intriguing possibility that N-acetylglucosamine may be a simple therapy to promote myelin repair in multiple sclerosis patients,” Demetriou added. Large well-controlled clinical trials are now needed to test this hypothesis.
The study, “N-Acetylglucosamine drives myelination by triggering oligodendrocyte precursor cell differentiation,” was published in the Journal of Biological Chemistry.
In the brain, myelin damage attracts immature, stem-like cells called oligodendrocyte precursor cells (OPCs) to the lesion site, where they mature into oligodendrocytes — myelin-producing cells capable of restoring the myelin sheath.
Despite the presence of OPCs in MS lesions, remyelination (myelin repair) is incomplete or absent. As such, increasing efforts are focused on identifying potential therapeutic approaches to promote oligodendrocyte maturation and/or remyelination.
Read more articles about myelin
Researchers at UCI, along with colleagues in Canada and Germany, now have identified GlcNAc as one of these potential approaches.
GlcNAc is a simple sugar that works as a building block of complex sugar molecules and glycoproteins (proteins containing sugar molecules). GlcNAc branching is involved in several cellular processes, including signaling and maturation.
This sugar is found in several body fluids, including breast milk, and is sold as an over-the-counter dietary supplement to manage joint pain, inflammatory bowel disease, and to prevent heart disease and stroke. Clinical evidence supporting its benefits are scarce, however.
Previous studies in mouse models of MS showed that GlcNAc branching deficiency promotes T-cell-mediated myelin loss and neurodegeneration, whereas oral treatment with GlcNAc suppresses inflammatory T-cell responses and MS-like disease when initiated after disease onset. Of note, T-cells are a type of immune cell involved in the abnormal attacks against myelin seen in MS.
In the present study, the team found that adding GlcNAc to mouse OPCs grown in the lab promoted their maturation into oligodendrocytes and myelin production. This process was dependent on GlcNAc branching and on the levels of PDGFR-alpha (involved in OPCs’ differentiation) on the surface of OPCs.
Similar results were observed in newborn pups receiving GlcNAc through their mothers’ breast milk following GlcNAc treatment in drinking water.
In a mouse model of MS, oral treatment with GlcNAc also drove oligodendrocytes maturation and myelin production, preventing myelin and nerve fiber damage, as well motor function loss.
The team next assessed whether GlcNAc blood levels were associated with brain lesions in 180 people with MS.
Data showed that patients with low GlcNAc levels had significantly greater myelin and nerve fiber damage, suggesting that “N-acetyglucosamine deficiency may contribute to disease severity,” said Alexander Brandt, MD, who led the clinical parts of the study.
Low GlcNAc levels also were linked to “a progressive disease course, clinical disability, and multiple neuroimaging measures of neurodegeneration,” the researchers wrote, noting that these particular data remain unpublished.
“The mechanisms that drive neurodegeneration in MS are poorly understood and our data raise the possibility that alterations in [GlcNAc] branching and/or GlcNAc availability may promote neurodegeneration by blocking remyelination,” the team wrote.
“GlcNAc is also known to be highly safe in humans,” the researchers added, noting that “coupled with availability as a dietary supplement, oral GlcNAc may provide a potent, inexpensive and safe therapy for MS.”
Michael Sy, MD, PhD, the study’s first author, added: “since N-acetylglucosamine is a major component of human breast milk but not baby formula, it may explain some of the cognitive function and myelination benefits realized by children fed breast milk as opposed to formula.”
Sy also is an assistant professor of neurology at UCI School of Medicine and the co-director of the MS program at the VA Long Beach Healthcare System.
Future clinical studies are needed to confirm the therapeutic potential of oral GlcNAc in this patient population.