Myelin Restored on Regenerated Optic Nerve Fibers of Mice in Study
Written by |
Using a two-pronged approach, researchers were able to restore myelin on regenerated nerve fibers in a mouse model of optic nerve injury, which has implications for multiple sclerosis (MS) and other diseases associated with myelin loss, a study reported.
The study, “Robust Myelination of Regenerated Axons Induced by Combined Manipulations of GPR17 and Microglia,” was published in the journal Neuron.
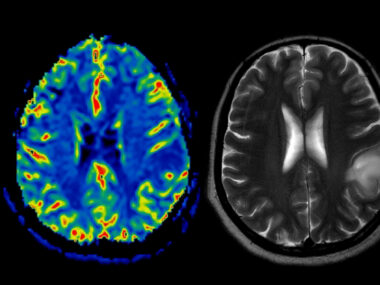
The hallmark of MS is the loss of the myelin sheath — a fatty protective coating surrounding the fibers, or axons, of nerve cells (neurons). Without myelin, electrical impulses traveling along axons are slower and less efficient, leading to nerve cell degeneration in the central nervous system (CNS, brain and spinal cord) and a range of disease symptoms.
In an earlier study, researchers at Boston Children’s Hospital, working in a mouse model optic nerve damage, discovered several treatments that promoted the regeneration of damaged axons, but did not restore optic nerve function. The team found that these regenerated axons did not regenerate myelin, similar to what occurs in advanced stages of MS.
To understand why this happens, these same researchers continued their work in mouse models of optic nerve injury “to uncover the regulatory mechanisms of myelination after CNS injury,” they wrote in the new study.
Myelination is carried out in the brain by cells known as oligodendrocyte precursor cells (OPCs). Three to five days after optic nerve injury to the mice, the growth of OPCs increased significantly in response, before returning to normal levels.
OPC transformation, or differentiation, into fully functioning myelin-producing cells was also blocked, resembling what occurs in lesions in progressive MS patients.
MS brain lesions are “similar to what we see in the optic nerve after injury,” Zhigang He, PhD, with the F.M. Kirby Neurobiology Center at Boston Children’s, said in a press release. “Both suffer from myelination failure so we believe our results could have some implications for new MS treatments, particularly for progressing MS.”
“We found that in injured optic nerves, OPCs fail to differentiate into mature myelination-competent oligodendrocytes,” he added.
To understand how OPCs fail to differentiate into myelin-producing cells after an injury, the researchers tested various compounds shown to promote OPC growth and differentiation in mice over four weeks after optic nerve injury.
A compound called montelukast was the strongest at stimulating OCPs into myelin-producing cells. This compound is known to block the protein GPR17, and is an anti-inflammatory medicine approved to treat asthma and seasonal allergies.
Further experiments showed GPR17, which was significantly overexpressed in injured nerves, prevented OPCs’ early differentiation into immature oligodendrocytes, which further progress to mature myelin-producing cells. Blocking this protein, however, failed to promote late-stage maturation of these cells.
As nerve cell inflammation has been shown to regulate OPC growth, researchers then investigated immune cells called microglia, which act as the immune defense in the CNS. Experiments found sustained activation of microglia after injury was able to suppress different stages of OPC differentiation.
When microglia cells were removed a few days before injury using a compound called PLX3397, OPC growth was also suppressed, suggesting these cells were needed for OPC growth.
However, when this treatment was given two weeks after injury, OPCs were able to proliferate in response to the injury, and there was an increase in the number and proportion of mature myelin-producing oligodendrocytes.
Based on these results, mice were treated with montelukast to block GPR17 for four weeks after optic nerve injury, or PLX3397 to suppress microglia cells for two weeks, starting two weeks after injury.
Montelukast treatment alone resulted in the myelination of about 15% of damaged nerve cells, while PLX3397 alone increased myelination in 21% of axons. Myelin structures were also noticeably thinner after montelukast treatment, “consistent with our results showing that this compound promotes generation of early differentiated OPCs,” the researchers wrote.
In mice treated with both montelukast and PLX3397, 60% of regenerated axons were myelinated. While these myelin structures were still thin, the researchers suggest this was due to “ongoing myelination.”
“In a mice model of optic nerve injury, we found that when we combined treatment of montelukast and removing microglia later after injury, the majority of axons could be remyelinated,” He said. “We believe that this work represents an important step towards functional restoration of cells in the adult central nervous system.”
“Future studies will examine whether such treatments enhance behavioral improvements in injury models and other pathological conditions,” the research team wrote.