Inflammatory Immune Cells Found in Active, But Not Chronic, Brain Lesions
Written by |
A class of immune cells called myeloid cells that express the inflammatory protein SIGLEC1 may be able to distinguish between active and chronic multiple sclerosis (MS) brain lesions, a study found.
The study, “SIGLEC1 (CD169): a marker of active neuroinflammation in the brain but not in the blood of multiple sclerosis patients,” was published in Scientific Reports.
MS and neuromyelitis optica spectrum disorder (NMOSD) are autoimmune disorders that result from the body’s immune system erroneously attacking its own cells, leading to inflammation in the central nervous system.
SIGLEC1 is an immune protein whose production is induced by the presence of type I interferons, which are proteins that are secreted by immune cells and used to treat relapsing-remitting MS (RRMS).
Myeloid cells, a group of immune cells involved in innate immune responses, expressing SIGLEC1 have been observed in mouse and human MS brain lesions, and elimination of these cells alleviated signs of disease in a mouse model of MS.
A team of researchers in Germany sought to determine if SIGLEC1 could act as a marker for MS or NMOSD activity by analyzing its expression in immune cells and lesion tissue.
Their analysis involved a total of 158 participants, including 86 MS patients, 41 NMOSD patients, and 31 healthy controls.
Initial results showed that 18.6% of the MS patients, 9.8% of NMOSD patients, and 3.2% of controls had high levels of SIGLEC1 in a type of myeloid cells called monocytes. However, for most MS patients (68.6%), this protein was elevated because they were receiving interferon beta as a treatment for their condition, which is known to raise SIGLEC1 levels.
Overall, there were three RRMS patients and two with primary or secondary progressive MS who had elevated levels of SIGLEC1 on monocytes, but were not on interferon beta treatment. These levels, however, did not correlate with disability scores or relapses.
Only one NMOSD patient had elevated SIGLEC1, which was explained by the presence of a concurrent mixed connective tissue disease that has been linked to increased type 1 interferon activity.
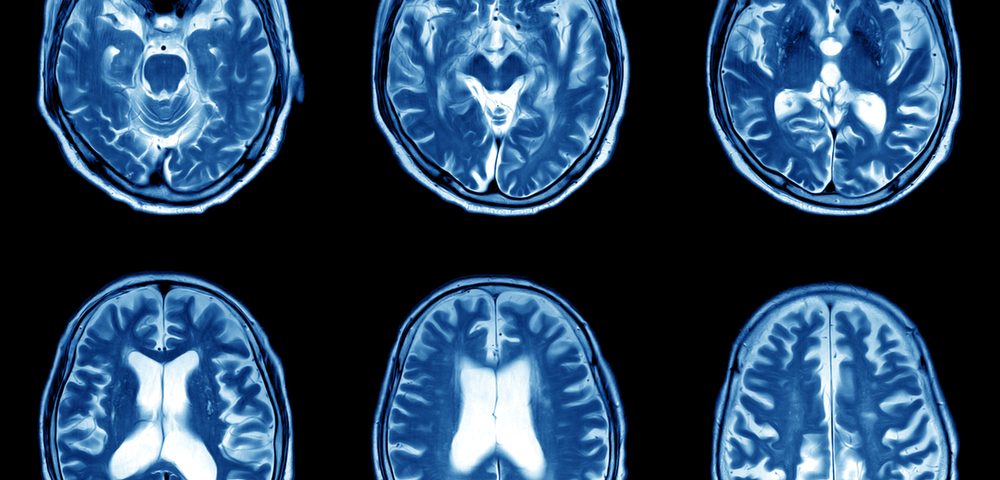
The researchers then examined the presence of SIGLEC1-positive cells in brain tissue samples from four MS patients with suspected active MS lesions and from five secondary progressive MS patients with chronic lesions. Six non-MS patients who died of cardiovascular disease were used as controls.
In control brains, SIGLEC1-positive cells were found only in macrophages — a kind of myeloid cell that engulfs pathogens — in the periphery of blood vessels and in the meninges, which are layers that surround the brain and spinal cord.
However, there was a remarkable infiltration of SIGLEC1-positive myeloid cells into acute MS brain lesions. Of note, patients with chronic lesions also had a high number of myeloid cells in their lesions, but most of these cells were not producing the SIGLEC1 protein.
The findings suggested that myeloid cell SIGLEC1 expression could be a potential biomarker to differentiate active and chronic lesions in people with MS.
SIGLEC1-expressing myeloid cells also were observed in brain tissue from patients with multiple inflammatory nervous system diseases, including stroke, glioblastoma, and encephalitis (brain inflammation) caused by herpes simplex.
“SIGLEC1+ myeloid cells in the brain are present in active inflammatory MS lesions as well as in other inflammatory neurological diseases,” but not in chronic MS lesions, the research team concluded, noting that the MS patients “did not have increased expression of SIGLEC1 on monocytes in the peripheral [circulating] blood.”
The study was limited by the inclusion of patients with relatively low disease activity and the use of immunosuppressive therapies in most.
“Future studies in MS and NMOSD patients during a clinical relapse could … still discover the presence of SIGLEC1 expressing monocytes in the peripheral blood,” the researchers added.


