High Free Light Chains Levels May Indicate Sooner Second Relapse
Written by |
High levels of kappa-free light chains, or kappa-FLC, in the cerebrospinal fluid (CSF) — the liquid surrounding the brain and spinal cord — may help identify people with clinically isolated syndrome (CIS) who will progress sooner to multiple sclerosis (MS), a study reports.
Overall, those with a high kappa-FLC index — a ratio of CSF to blood levels — were twice as likely to experience a second relapse and progress to overt MS within 12 months than patients with a low index.
Given these findings, the researchers say this index may serve as a biomarker to determine which patients will benefit the most from early treatment to delay MS progression and disability accumulation. Indeed, the index could replace other indicators, “taking us one step closer to tailored medicine in MS,” the scientists said.
The study, “Kappa-Free Light Chains in CSF Predict Early Multiple Sclerosis Disease Activity,” was published in Neuroimmunology and Neuroinflammation.
The first clinical manifestation of relapsing MS — when patients have clear symptoms of the neurodegenerative disorder — is called CIS. With CIS, patients have evidence of a first demyelinating event, or an immune attack to the myelin sheath surrounding nerve fibers, and causing symptoms, that lasts at least 24 hours.
A majority of CIS patients will experience a second relapse and convert to overt relapsing-remitting MS in their lifetime.
Early treatment with disease-modifying therapies, called DMTs, can delay the onset of MS and prevent a second neurologic episode. However, knowing which patients will experience a second attack or relapse sooner — and therefore experience more long-term disability — is key to determining who will benefit from early treatment.
“In clinical practice, the benefit of a reliable biomarker — either singular or in combination with others — is that patients with early MS with a higher risk for further disease activity, that is, e.g., shorter time to a second attack, could be advised to start DMT early or use highly effective DMT,” the researchers wrote.
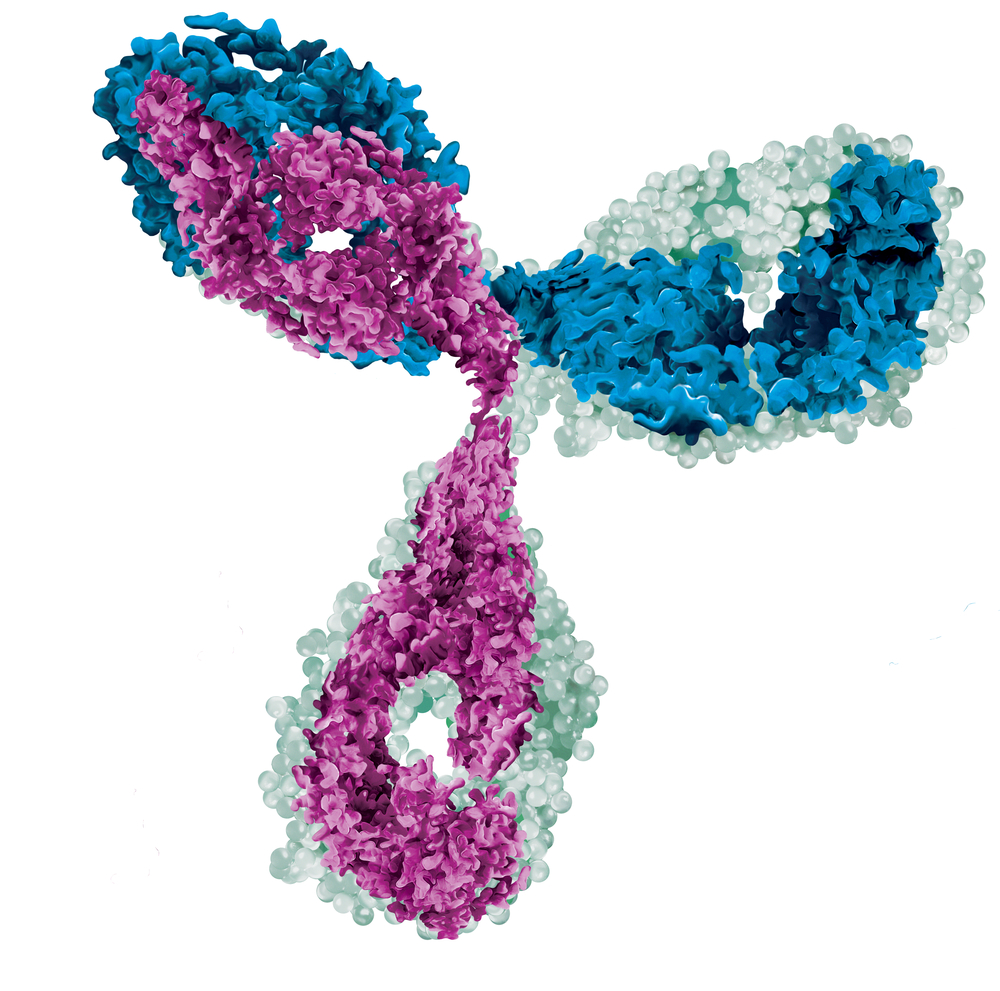
Light chains are proteins made by plasma cells that typically combine with other proteins called heavy chains to produce antibodies. Of note, antibodies are blood proteins that attack bacteria, viruses, and other foreign invaders in the blood. When not combined with heavy chains, they are released into the bloodstream and called free light chains or FLCs.
Previous studies have shown that FLC levels in the CSF are more accurate indicators of multiple sclerosis than are oligoclonal bands or OCBs. OCBs are bands of proteins called immunoglobulins that indicate inflammation of the central nervous system. However, it remains unclear if FLCs can predict MS severity.
To learn more, researchers in Austria now investigated whether the kappa-FLC index could predict disease activity in people with early MS, independently of other clinical and demographic characteristics.
A total of 88 patients (68% female), with a mean age of 33, were included in the study. At its start, almost all participants had experienced symptoms consistent with damage to a single brain region, typically inflammation of the spinal cord (45%), optic nerves (30%), or the brainstem/cerebellum (24%).
The cerebellum is a structure of the central nervous system that controls movement, and the brainstem is important to convey motor and sensory signals between the brain and the rest of the body.
Over a median follow-up of 47 months (nearly four years), 38 patients progressed to clinically definite MS, or CDMS. In addition, 20 participants received early DMT — before progressing to definite MS among those who converted and during follow-up for those who did not.
At baseline, or the study’s start, the median kappa-FLC index was 36.5, and 76 patients were considered positive, meaning that their index was 6.6 or higher. Essentially, a positive index is indicative that kappa-FLC is being produced by immune cells in the brain and spinal cord.
The results showed that patients with a higher kappa-FLC index at disease onset were significantly more likely to convert to definite MS earlier than those with lower index scores.
For each 10-point rise in the kappa-FLC index, participants had a 13% higher risk for progression to MS, even when taking into account variables such as age, sex, number of brain lesions, disease duration, and use of DMT.
The participants were then divided into two subgroups: one included patients with a high index (above 100) and the other, those with a low index (100 or lower).
Those with high scores at disease onset were twice as likely to experience a second relapse within one year, and four times more likely within two years. Overall, the median time to a second relapse was 11 months — or within one year —for patients with a high index, and 36 months (about three years) for those with a low index.
“Our cohort, which is representative for patients with a first demyelinating event, shows that an increase of κ [kappa]-FLC index by 10 indicates an increased risk by approximately 13% for a second clinical attack,” the researchers wrote.
The team noted that measuring the kappa-FLC index might have greater prognosis value than using oligoclonal bands. This is not only because the kappa-FLC index uses a much cheaper and easier to implement method, but also because it returns a metric result covering a range from approximately 1 up to 500, the researchers said.
In contrast, “OCB status is dichotomous, returning either a positive or negative result as assessed by visual inspection,” they wrote.
Limitations of the study included long-term sample storage before analysis and the collection of CSF and blood samples after participants had received steroids. However, the researchers said that “the effect of freezing on FLC concentrations (at -20°C) has been reported to be irrelevant.” Also, while high-dose steroids can lower blood FLC concentrations, it does not affect CSF levels or calculations of the FLC index.
“κ-FLC is a reliable prognostic biomarker that might replace OCB determination taking us one step closer to tailored medicine in MS,” the team said. However, they added that “further studies in a multicenter setting including higher number of patients are required” to confirm these results across a broader patient population.


