Cholesterol Made by Nerve Cells Repairs Myelin Damage in Mice
Written by |
Cholesterol made by neurons is crucial for repairing long-term damage to the myelin sheath, the fatty coating around nerve fibers that is damaged in multiple sclerosis (MS), according to a new report based on experiments done on mice.
The finding suggests that increasing neuronal cholesterol synthesis may be helpful in treating MS.
The study, “Neuronal cholesterol synthesis is essential for repair of chronically demyelinated lesions in mice,” was published in Cell Reports.
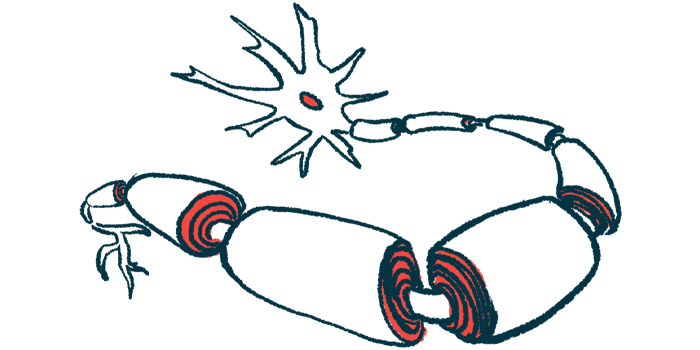
The myelin sheath is a fatty substance that wraps around the projections of nerve cells and helps them send electrical signals more efficiently, akin to rubber insulation around a metal wire.
MS is caused by the immune system erroneously attacking and damaging the myelin sheath. Remyelination — restoration of lost myelin — is widely considered a “holy grail” for treating MS. However, little is understood about exactly how remyelination happens in the body, which has made it difficult to develop treatments. So far, there are no approved MS therapies that target remyelination.
One of the main components in the myelin sheath is cholesterol, which accounts for more than one quarter of all the fats found in myelin.
When damaged myelin is repaired, new cholesterol must be incorporated in it, and prior research has suggested that where the cholesterol comes from differs based on the type of damage. In acute myelin damage, cholesterol from the damaged myelin is “recycled” to make new myelin. By contrast, in chronic damage, this recycling is impaired over time, so cells must instead make new cholesterol.
This raises the question of exactly which cells are generating that cholesterol. Normally, most myelin is manufactured by a class of supporting cells called glia, which includes astrocytes and oligodendrocytes, among others.
Here, through experiments in mice, a team led by scientists in Germany demonstrated that, while glia do produce a substantial amount of cholesterol (in support of their myelin-making activities), neurons also have the capacity to make cholesterol. Furthermore, neuronal cholesterol production changed in response to myelin damage.
More specifically, in response to acute damage, neurons produced less cholesterol. However, several weeks after undergoing chronic damage, the neurons increased cholesterol production, which suggests “enhanced cholesterol synthesis in neurons during remyelination,” according to the researchers.
Additional experiments showed that remyelination after chronic injury was impaired in mice engineered so their neurons were unable to synthesize cholesterol.
Notably, the reduction in neuronal myelin production was accompanied by reduction in a type of glial stem cell called oligodendrocytes precursor cells (OPCs). OPCs are crucial for remyelination, as these originate myelin-producing cells called oligodendrocytes.
“Together, these findings raise the possibility that elevating neuronal cholesterol synthesis is essential for OPC proliferation and differentiation [growth and development] to facilitate remyelination,” the researchers concluded.
In analyses of brain tissue from MS patients, the researchers found decreased expression of genes needed for cholesterol synthesis in neuronal lesions — that is, damaged neurons. By contrast, healthy neurons in MS brains had increased expression (activity) of these genes, “suggesting increased neuronal cholesterol synthesis in normal-appearing MS tissue areas,” the researchers wrote.
“Taken together, our data show that loss of neuronal cholesterol synthesis strongly impairs remyelination with relevance for human MS disease,” the scientists concluded, noting a need for more research into ways to stimulate cholesterol production in damaged neurons.
“The challenge of the next studies will be to develop therapy concepts for patients with myelin disorders in which acute and chronic lesions can be treated simultaneously,” Gesine Saher, PhD, a co-author of the study from the Max Planck Institute for Experimental Medicine in Germany, said in a press release.



