Rituximab for MS may safely control disease in children, teens
Use of off-label treatment found to reduce relapses, new lesions: Study
Written by |
Treatment with rituximab, an approved CD20 inhibitor that’s sometimes used off-label for multiple sclerosis (MS), was found to adequately control the neurodegenerative disease in patients diagnosed during childhood or adolescence, a new study showed.
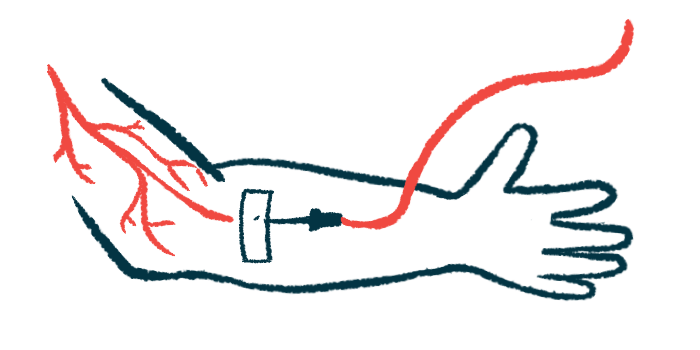
The therapy, given by infusion into the bloodstream, was generally safe and significantly reduced the rate of relapses and the number of new lesions among patients diagnosed as children or teenagers, data showed. Over about 20 months of follow-up, a total of 70% of patients still had no evidence of disease activity, defined as no relapses, no new MRI activity, and no disability progression.
“Our data underline that [rituximab] is a treatment strategy with an excellent risk-benefit profile in pediatric MS patients at risk for unfavorable disease outcomes,” the researchers wrote in their study, “Rituximab treatment in pediatric-onset multiple sclerosis,” which was published in the European Journal of Neurology.
While MS generally develops in individuals between the ages of 20 and 40, a small proportion of patients — about 2% to 5% — experiences their first symptoms before reaching adulthood. In these cases, the disease is called pediatric MS or pediatric-onset MS (POMS).
These patients exclusively have relapsing-remitting MS (RRMS), which is defined by sudden periods of new or worsening symptoms, called relapses, followed by periods of remission when symptoms ease. Although RRMS is also the most common form of MS in adults, POMS patients tend to have a higher relapse rate and inflammatory activity, and experience greater disability at a younger age.
Few disease-modifying therapies tested in clinical trials to date
It’s becoming increasingly evident that starting patients on high-efficacy disease-modifying therapies (DMTs) as early as possible leads to better outcomes in the long term — both in adults and in children and adolescents with MS. These therapies can reduce the rate of relapses, and also significantly delay the progression of disability, sometimes by several years.
“However, only [a] few disease-modifying therapies (DMTs) approved for adults have been investigated in randomized controlled trials in the pediatric MS population and access to treatment is highly variable around the globe,” the researchers wrote.
A number of CD20 inhibitors, such as Ocrevus (ocrelizumab), Kesimpta (ofatumumab), and Briumvi (ublituximab), are now widely approved for adults with MS. Children and adolescents with the disease, however, have limited access to them.
Rituximab is another anti-CD20 antibody that is sometimes used as a treatment for people with MS. It is not approved to treat MS, but many healthcare practitioners prescribe it off-label to reduce disease activity and disability progression in both adults and children with MS.
Now, a group of researchers set out to describe the risk-benefit profile of rituximab in children and teens with MS. They examined data from 61 patients diagnosed between 2009 and 2022 at centers in Sweden, Austria, and Germany, all of whom received the medication before the age of 19.
These pediatric patients had a mean age of 14.9 at the time of their first symptoms, and were 15.2 years old, on average, at diagnosis. More than two-thirds (69%) received rituximab as their first DMT, but some had been given other MS therapies before it. Specifically, about 25% had received one prior therapy while about 5% had received two; nearly 2% had received three.
Use of rituximab for MS may help ‘particularly vulnerable’ patients
Overall, the median time from the first symptom to starting the first DMT was 150 days, or about five months. Meanwhile, those taking rituximab started treatment at a median of 240 days, or about eight months. The most common rituximab treatment regimen was one initial dose of 500 or 1,000 mg, which was then repeated every six months.
After a median of 20.9 months, or just longer than 1.5 years, the number of relapses per year had significantly decreased from 0.6 to 0.03 during rituximab treatment, with the majority of the patients (90%) remaining relapse-free, the results showed.
Significant reductions also were observed in disease activity seen on MRI scans. The data showed the annual rate of total new lesions dropped from 1.25 to 0.08, and the number of new lesions with active inflammation was reduced from 1.25 to zero.
Disability levels, as assessed with the Expanded Disability Status Scale (EDSS), also decreased from a score of one before treatment initiation to zero at the last follow-up, indicating an overall easing of symptoms.
Finally, 70% of the patients retained a status called no evidence of disease activity, or NEDA-3, which is marked by the absence of relapses, new or enlarging lesions, and sustained increases in EDSS scores.
[Use of rituximab] as a first-line agent, as seen in 69% of our patients, may prevent patients from the medical, social, and emotional consequences of ongoing disease activity and reduce the risk of future disability in this particularly vulnerable population.
Adverse events were reported in 67% of patients, and were mainly mild to moderate. The most frequently reported events were infusion-related (48%), followed by infections (20%), low levels of antibodies (17%), and low levels of immune cells called lymphocytes (7%).
While most patients (90%) remained on the treatment during the study period, four individuals discontinued the therapy due to adverse events, and two due to ongoing disease activity.
“Our data suggest that [rituximab] is an effective and safe treatment option in POMS when applied both as [a] first-line therapy and as a rescue therapeutic option,” the researchers wrote.
The team noted, moreover, that the use of rituximab for MS “as a first-line agent, as seen in 69% of our patients, may prevent patients from the medical, social, and emotional consequences of ongoing disease activity and reduce the risk of future disability in this particularly vulnerable population.”


