Rituximab as effective as Ocrevus as RRMS treatment: Study in Egypt
Using less-costly drug may help 'overcome the cost barrier' to treatment
Written by |
Rituximab, sometimes used off-label as a multiple sclerosis (MS) treatment, may be as effective — at a much lower cost to patients — as the approved therapy Ocrevus (ocrelizumab) at managing relapsing forms of the disease, a new study from Egypt suggests.
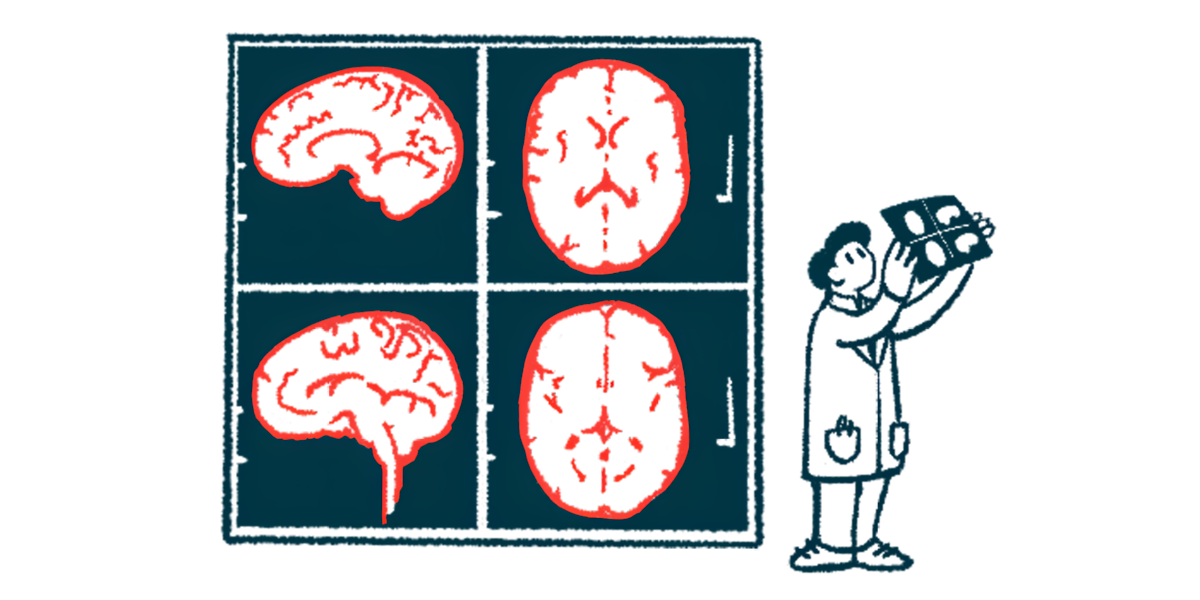
The study’s results showed that the two therapies demonstrated similar efficacy in people with relapsing-remitting multiple sclerosis (RRMS), a disease form in which relapses are interspersed with periods of remission. Both treatments were found to reduce the number of relapses, prevent changes seen on brain scans linked to MS activity, and slow disability accumulation among patients.
Still, infusion-related reactions were significantly more common with rituximab, the researchers noted.
According to the team, these results suggest that rituximab — which is widely available and has many biosimilars, or products similar to generics — may represent a cheaper option for people who cannot access or cover the cost of approved medications such as Ocrevus. This may especially be the case for RRMS patients in developing countries such as Egypt, the researchers noted.
“No difference in efficacy was found between [Ocrevus] and rituximab in treating RRMS,” the researchers wrote. “The utilization of the cheaper of the two medications … could help to overcome the cost barrier,” resulting in a “better outcome in patients with RRMS.”
The study, “Efficacy of ocrelizumab versus rituximab in patients with relapsing remitting multiple sclerosis,” was published in the journal Acta Neurologica Belgica.
Comparing outcomes of rituximab vs. Ocrevus treatment
Anti-CD20 antibodies such as Ocrevus and rituximab are a class of disease-modifying therapies (DMT) that aim to reduce inflammation and MS-related damage by depleting immune B-cells, which are key drivers of MS.
Ocrevus is one of the three CD20 inhibitors approved for relapsing forms of MS. Rituximab is an anti-CD20 antibody that was developed before any of the currently approved therapies. It was originally designed to treat B-cell cancers, and has shown promise in MS clinical trials, but its development for MS was halted when new therapies started to emerge.
“Despite the promising results, clinical development of [rituximab] was interrupted, probably due to the emergence of newer B-cell-depleting therapies (Ocrevus),” the researchers wrote.
Rituximab remains a common alternative to other CD20 inhibitors in many countries due to its lower cost; the treatment also has a favorable efficacy and safety profile. However, clinical trials directly comparing rituximab with approved anti-CD20 therapies in MS patients are still ongoing.
To directly compare the two therapies, the team, led by scientists at Cairo University, examined data from 126 RRMS patients, ages 18-60. Each had received either rituximab or Ocrevus for at least one year while being treated at the university’s Kasr Al-Ainy MS unit from August 2022 to April 2023. About half of the patients received Ocrevus, while the other half had been given rituximab.
Before starting treatment, the groups were fairly similar in terms of age, disease duration, disability levels, disease activity, and proportion of patients who had received a previous DMT.
More side effects seen with use of off-label therapy
The mean treatment duration was about 18 months for patients on Ocrevus and 21 months for those on rituximab. According to the researchers, no significant differences in key clinical outcomes were observed between the two groups.
The majority of patients had stable disability levels, as assessed by Expanded Disability Status Scale (EDSS) scores. About 9.4% of patients on Ocrevus and 11.3% of those on rituximab experienced a three-month confirmed disability worsening, or CDW, defined as an increase in EDSS scores sustained for at least three months. The proportion of patients with a confirmed disability improvement was also similar between the groups (21.8% vs. 30.6%).
Significant and similar reductions in MS relapse rates were seen with both therapies: Those on Ocrevus went from 1.4 relapses per year before treatment to 0.21 relapses per year while on the therapy, while those on rituximab saw their relapses decrease from 1.33 to 0.29 per year.
These results are very important for MS practice in developing countries with suffering economies like Egypt considering the increasing costs of MS treatments, especially monoclonal [antibodies] like [Ocrevus].
Patients on Ocrevus took longer to experience a first CDW event (42.6 vs. 34.8 months) or a first relapse (36.1 vs. 24.5 months), the data showed. However, these differences were not statistically significant, per the researchers.
MRI findings, including the presence of new or enlarging lesions and lesions with active inflammation, were also similar between the two groups, though the researchers noted this finding should be interpreted with caution. Many follow-up MRI studies were incomplete, and imaging was performed at different centers, which may limit the ability to make accurate and objective comparisons between the groups.
“This study demonstrates that there is no significant difference in the effectiveness of [Ocrevus] and rituximab in controlling disability accumulation, relapse activity, and MRI activity among patients with relapsing-remitting multiple sclerosis,” the researchers wrote.
Because both Ocrevus and rituximab are administered through intravenous, or into-the-vein, infusions, infusion-related reactions are a known potential side effect. These reactions were more significantly frequent with rituximab (59.7% vs. 42.2%). Infection rates, however, were comparable between the two treatments.
“These results are very important for MS practice in developing countries with suffering economies like Egypt considering the increasing costs of MS treatments, especially monoclonal [antibodies] like [Ocrevus],” the team concluded.