Types of multiple sclerosis
What are the four types of MS?
Multiple sclerosis (MS) is a neurological disorder in which an erroneous inflammatory attack by the body’s immune system causes the loss of an insulating cover, called the myelin sheath, around nerve fibers.
Damage to or the loss of myelin leads to impaired nerve function in the brain and/or spinal cord, ultimately resulting in the disease’s symptoms. MS symptoms vary greatly among patients, depending on which parts of the nervous system are most affected.
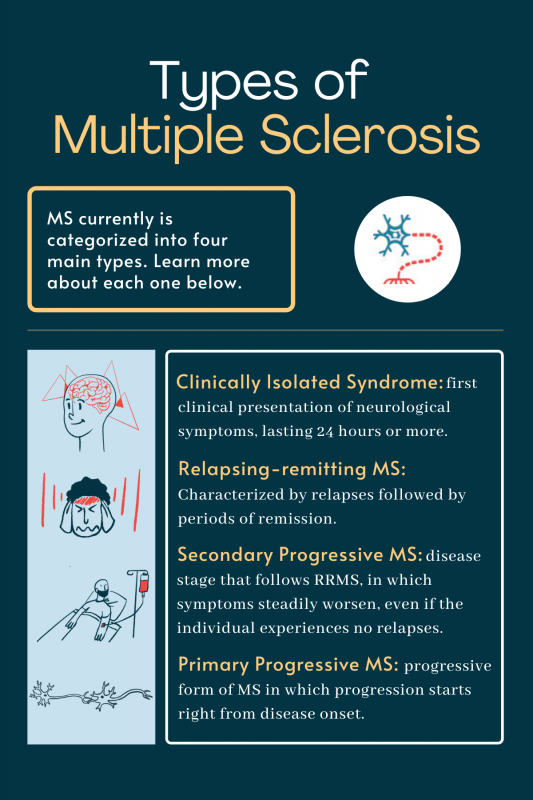
Based on work from the National MS Society Advisory Committee on Clinical Trials of New Agents in MS and the International Advisory Committee on Clinical Trials in MS, MS currently is categorized into four main types. These MS types depend on the disease’s clinical presentation and include:
- clinically isolated syndrome
- relapsing-remitting MS
- secondary progressive MS
- primary progressive MS
There also are rarer MS subtypes and MS-like disease.
Clinically isolated syndrome
Clinically isolated syndrome (CIS) is the first clinical presentation of neurological symptoms attributed to inflammation and loss of myelin in the central nervous system, or CNS, which includes the brain, spinal cord, and optic nerves. This episode must last 24 hours or more, and not be accompanied by fever or infection, to be considered a first presentation of the disease.
This form of MS can be classified as:
- monofocal: a single neurologic sign or symptom caused by a single lesion
- multifocal: refers to multiple symptoms caused by lesions in more than one CNS region
CIS can be thought of as a “single relapse” of MS, which means it is not technically MS. According to the 2017 McDonald criteria — a set of guidelines used to diagnose MS — the disease can only be diagnosed if patients have evidence of damage in multiple regions in the CNS, and if that damage occurred at different points in time.
An individual who has experienced a first episode of MS-like symptoms generally is considered to have CIS until physicians find more evidence of full MS. This evidence can occur either in the form of additional relapses or through the development of new brain lesions.
Some people with CIS never have another episode of symptoms nor develop more lesions, and thus never progress to clinically definite MS. Or individuals may experience another relapse and/or have evidence of additional lesions, and be diagnosed with the condition.
The likelihood that someone with CIS will eventually develop MS varies significantly based on the presence or absence of brain lesions on MRI scans. While people without clearly detectable brain lesions have an approximately 20% chance of progressing to MS, there is a 60–90% chance that CIS patients with brain lesions will progress to clinically definite disease.
These patients may be treated with disease-modifying therapies to delay the onset of MS.
Relapsing-remitting MS
The most common form of MS is relapsing-remitting MS (RRMS), which is estimated to account for about 85% of all newly diagnosed cases.
This form of the disease is characterized by relapses (also called exacerbations), which are defined by the appearance of new symptoms or the worsening of old symptoms for 24 hours or more, without a change in body temperature or an infection.
These relapses are followed by remissions, which are periods of partial or complete recovery from symptoms. During remissions, all symptoms may disappear or some may continue and become permanent. However, no apparent progression of the disease occurs during this time.
RRMS can be characterized by two aspects, which are not mutually exclusive:
- active or non-active disease, based on the occurrence of relapses and/or new brain lesions on MRI scans.
- worsening or not worsening, based on whether or not there is an incomplete recovery, or an increase in disability, following a relapse.
Biologically, RRMS differs from progressive types of MS because the relapses represent new inflammatory attacks on the brain and/or spinal cord. By contrast, much less inflammation is present in the progressive forms of the disease.
Secondary progressive MS
Secondary progressive MS (SPMS) is a disease stage that follows RRMS. With this type of MS, a person’s symptoms steadily worsen, even if the individual experiences no relapses.
Notably, disease exacerbations still may occur in SPMS. But symptom changes generally are much less drastic than in the RRMS stage. Also, symptoms do not completely disappear in the remission phases.
A diagnosis of SPMS usually comes after reviewing the progression of the disease over several months, though there is no single test that defines when the disease changes from RRMS to SPMS. SPMS also can be classified as:
- active or non-active, based on MRI evidence of increasing nervous system damage and/or occasional relapses.
- with or without progression, based on whether or not the individual experiences disability accumulation over time.
The time it takes to progress from RRMS to SPMS is different for everyone with multiple sclerosis. If the disease were left untreated, about 50% of patients would convert to SPMS within a decade, and 90% within 25 years.
But because of advancements in disease-modifying therapies (DMTs), fewer people today develop SPMS than ever before, and the transition tends to occur later in life. In fact, a recent study found that when most patients received treatment, it took a median of three decades for 1 in 10 patients to convert to SPMS.
The reasons why RRMS develops into SPMS are not fully understood, but the mechanisms of progression between these MS categories, or types, seem to differ.
In RRMS, symptoms are thought to be driven by active inflammation that causes damage in the brain. By contrast, SPMS is driven mainly by neurodegeneration — nerve damage that continually worsens over time — mostly without active inflammation.
Primary progressive MS
Primary progressive MS (PPMS) is a progressive form of the disease that is diagnosed in about 15% of MS patients.
Similar to SPMS, it also is characterized by symptoms that become worse over time, without periods of relapse and remission. However, disease progression starts right from disease onset — hence the term “primary” progressive.
Like other MS classifications, PPMS also can be classified as:
- active or non-active, based on MRI evidence of new lesions and/or whether the person experiences occasional relapses.
- with or without progression, based on whether the patient experiences disability accumulation that is sustained over a certain period of time.
People with PPMS typically have fewer brain lesions and less inflammation than people with RRMS; however, they usually have more spinal cord lesions. These patients tend to develop symptoms about one decade later than those with relapsing forms of MS. Generally, these are more difficult to diagnose and treat.
How to know what type of MS someone has
Multiple sclerosis classification is generally done by monitoring MRI changes and neurological symptoms. If a person experiences MS-like symptoms for the first time, they may be diagnosed with CIS.
RRMS
After a first episode, some patients may eventually meet the criteria for RRMS.
A diagnosis of RRMS is generally based on the McDonald criteria. RRMS can be diagnosed if an individual shows clear-cut evidence of MS-like brain lesions that develop at multiple points in time, and that affect more than one part of the CNS.
There are several ways through which an individual with CIS could transition to RRMS. If the person has symptoms or lesions involving only one CNS region, another disease relapse or new lesions involving a different region would be required to meet the criteria.
On the other hand, someone with evidence of damage in two CNS regions at the time of the CIS diagnosis would meet the criteria with another relapse or a new lesion, even if those did not involve a different region in the brain or spinal cord.
SPMS
After these MS stages, some patients with RRMS may start to experience continual disease progression, even in the absence of relapse activity — leading to a diagnosis of SPMS. There are no formal guidelines defining the transition from RRMS to SPMS. Instead, the diagnosis generally is made after a review of how symptoms have changed over time.
PPMS
For PPMS, a diagnosis also is done according to the McDonald criteria. Based on these guidelines, a person with PPMS must have one year of continual disease progression — worsening of neurological function without remission — and at least two of the following:
- one or more brain lesions recognized as typical of MS.
- two or more lesions in the spinal cord.
- evidence of immune system activity in the CNS (such as the presence of certain antibodies in the fluid around the brain and spinal cord).
Is MS treatment the same for each type?
Disease-modifying therapies, or DMTs, currently available for MS all broadly work by reducing the inflammatory attack that drives the disease. Active inflammation tends to play a much more pronounced role in the progression of relapsing forms of MS compared with progressive forms. Consequently, current therapies are generally more effective in patients with relapsing MS.
There are more than a dozen therapies approved in the U.S. to treat relapsing forms of MS, which generally encompasses CIS, RRMS, and active SPMS — that is, SPMS with relapses or evidence of new disease activity on MRI scans. Most of these medicines also are approved elsewhere in the world, though in some countries they may be indicated only for RRMS.
Far fewer treatments are available for MS patients who experience progressive disease without relapses. The only therapy approved in the U.S. to treat PPMS is Ocrevus (ocrelizumab). Similarly, just one DMT, mitoxantrone, is approved for active and non-active SPMS.
| Type | Frequency | Clinical presentation | Approved DMTs |
|---|---|---|---|
| Clinically isolated syndrome | About 3-4 of every 100,000 people are diagnosed with CIS per year; about 85% will develop true MS. | A first episode of MS-like neurological symptoms lasting at least 24 hours. | Aubagio, Avonex, Bafiertam, Betaseron, Copaxone, Extavia, Gilenya, Mayzent, Kesimpta, Ocrevus, Plegridy, Ponvory, Rebif, Tecfidera, Tysabri, Vumerity, Zeposia |
| Relapsing-remitting MS | Accounts for approximately 85% of MS patients. | Characterized by relapses, when new symptoms appear or existing ones worsen, and periods of remission. | Aubagio, Avonex, Bafiertam, Betaseron, Copaxone, Extavia, Gilenya, Kesimpta, Lemtrada, Mavenclad, Mayzent, mitoxantrone, Ocrevus, Plegridy, Ponvory, Rebif, Tecfidera, Tysabri, Vumerity, Zeposia |
| Secondary progressive MS | Most people with RRMS will eventually transition to SPMS. | Continual worsening of symptoms over time, even in the absence of relapses. | Active SPMS: Aubagio, Avonex, Bafiertam, Betaseron, Copaxone, Extavia, Gilenya, Kesimpta, Lemtrada, Mavenclad, Mayzent, mitoxantrone, Ocrevus, Plegridy, Ponvory, Rebif, Tecfidera, Tysabri, Vumerity, Zeposia Non-active SPMS: mitoxantrone |
| Primary progressive MS | Accounts for roughly 15% of MS patients. | Gradual worsening of symptoms from disease onset. | Ocrevus |
Rare forms of MS
Other terms are sometimes used to describe rare MS patterns and MS-like disease. These include:
Malignant MS
Malignant MS is a form of multiple sclerosis in which the disease progresses very rapidly with severe relapses. Patients with this form of MS typically require an aid, such as a cane, to walk 100 meters (328 feet) within five years of disease onset. Other names for this form are fulminant, Marburg, aggressive, or advanced MS.
Inactive MS
Inactive, or benign MS, is a variant of RRMS that shows little or no worsening over many years, though that could still change at a later date. A person is typically said to have this form if they have gone about 15 years or longer with few symptoms and little disability. Sometimes inactive multiple sclerosis is called “burned-out” MS, in which the disease progression appears to slow after a long period of worsening.
Pediatric-onset MS
While MS usually occurs in adults, it can affect individuals younger than 18, in which case it is referred to as pediatric MS or pediatric-onset MS (POMS). Children with POMS have RRMS exclusively and tend to have more frequent relapses than adults, although they also tend to recover from relapses more quickly.
Radiologically isolated syndrome
In some cases, a person will have evidence of brain lesions on MRI scans similar to those seen in MS but will not have overt symptoms of the disease. These cases are termed radiologically isolated syndrome (RIS).
Patients with RIS should be monitored, and may be diagnosed with MS later on, if more symptoms appear.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
FAQs about types of MS
In general, progressive forms of multiple sclerosis, specifically primary progressive or secondary progressive MS, are associated with faster disease progression and more rapid accumulation of disabling symptoms than relapsing-remitting MS. However, this varies substantially between individuals.
While multiple sclerosis affects everyone differently, patients with relapsing-remitting multiple sclerosis (RRMS) tend to experience a slower accrual of disabling symptoms than those with progressive forms. RRMS patients also experience remissions, or periods between exacerbations where symptoms disappear or ease considerably. However, this can vary substantially between individuals.
All forms of multiple sclerosis can cause symptoms that make activities of daily life harder to do independently. In general, disability progression occurs more rapidly in progressive than in relapsing forms of the disease, but there is substantial variation in progression patterns from person to person.
The most common form of multiple sclerosis is relapsing-remitting disease, or RRMS. About 85% of patients are first diagnosed with this MS type.
Actress Selma Blair, TV talk show host Montel Williams, and Ann Romney, author and the wife of Utah senator Mitt Romney, were all initially diagnosed with relapsing-remitting multiple sclerosis, the most common form of the disease.
 Fact-checked by
Fact-checked by