#AAN2018 – Stem Cell Transplant is Effective Treatment for ‘Aggressive’ MS, Study Shows
Written by |
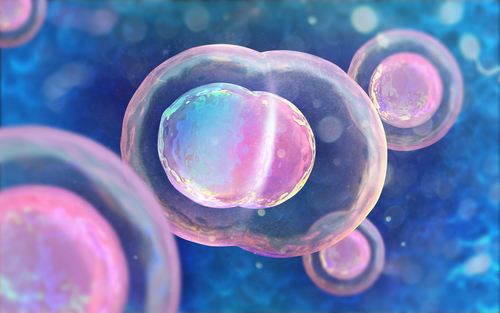
Autologous hematopoietic stem cell transplantation (aHSCT) has been shown to be safe and highly effective to treat patients with “aggressive” multiple sclerosis (MS). Tested in 19 patients, transplantation of stem cells was found to induce clinically meaningful improvements in disability.
These findings were shared at the 2018 Annual Meeting of the American Academy of Neurology (AAN) in Los Angeles, California, in a presentation titled “Autologous Haematopoietic Stem Cell Transplantation in Treatment Naïve Patients with ‘Aggressive’ Multiple Sclerosis.”
aHSCT uses a patient’s own healthy bone marrow stem cells, in combination with a much less aggressive chemotherapy and/or radiation regimen, to prepare the patient for the transplant.
Previous studies have suggested that aHSCT is an effective strategy to treat patients with highly active relapsing-remitting MS (RRMS) who do not respond to available disease-modifying therapies (DMTs), and international guidelines advocate for its use in patients with “aggressive” MS.
To further demonstrate the potential of aHSCT as a treatment for “aggressive” MS, a research team evaluated its safety and effectiveness in MS patients who had not been treated previously with DMTs.
A total of 19 patients were treated across several clinical centers: seven patients were from Sheffield, U.K., seven from Uppsala, Sweden, four from Ottawa, Canada, and one patient was from Florence, Italy. All patients received aHSCT between May 2004 and May 2017.
In addition to aHSCT, patients were treated with BEAM (carmustine, etoposide, cytarabine, melphalan) chemotherapy plus antithymocyte globulin (ATG) to reduce transplant rejection, or with Cytoxan (cyclophosphamide) with ATG, or the triple combination of Cytoxan, ATG, plus busulfan as conditioning regimens.
Patients had a median age of 33 years at diagnosis and received the aHSCT by a median time of nine years after symptom onset. They had a median disability score of 6.5 before the treatment, as determined by the Expanded Disability Status Scale (EDSS).
After a median follow-up period of 30 months, patients had a median EDSS score of 2.0, which represented a median improvement of 2 points (the higher the score, the worse the patient’s disability level).
None of the patients had clinical relapse following the transplant of stem cells.
Only three patients developed new brain lesions detectable by magnetic resonance imaging (MRI) at the first six-month follow-up evaluation, but no additional new lesions were detected in the following scans.
The adverse effects reported during the study were comparable to those previously observed in similar treatments. No deaths related to the treatment were reported.
Based on these preliminary results, the researchers concluded that aHSCT is “safe and highly effective in inducing rapid and sustain remission” in highly active MS, and “was associated with a significant improvement of [patient’s] level of disability.”
“aHSCT should be considered as first line therapy in patients with ‘aggressive’ MS,” the team concluded.
Another study presented at the AAN 2018 meeting further supports these findings, demonstrating the superior effectiveness of aHSCT over conventional DMTs for RRMS.