Small Molecule TDP6 Activates Myelin Regeneration in Mice with MS, Other Diseases, Study Finds
Written by |
A small synthetic molecule called TDP6 mimics a natural growth factor and promotes myelin regeneration in a mouse model of demyelination diseases such as multiple sclerosis (MS), a new study from Australia shows.
TDP6 works by targeting a receptor at the surface of myelin-producing cells called oligodendrocytes.
The study, “Targeting TrkB with a brain-derived neurotrophic factor mimetic promotes myelin repair in the brain,” was published in The Journal of Neuroscience.
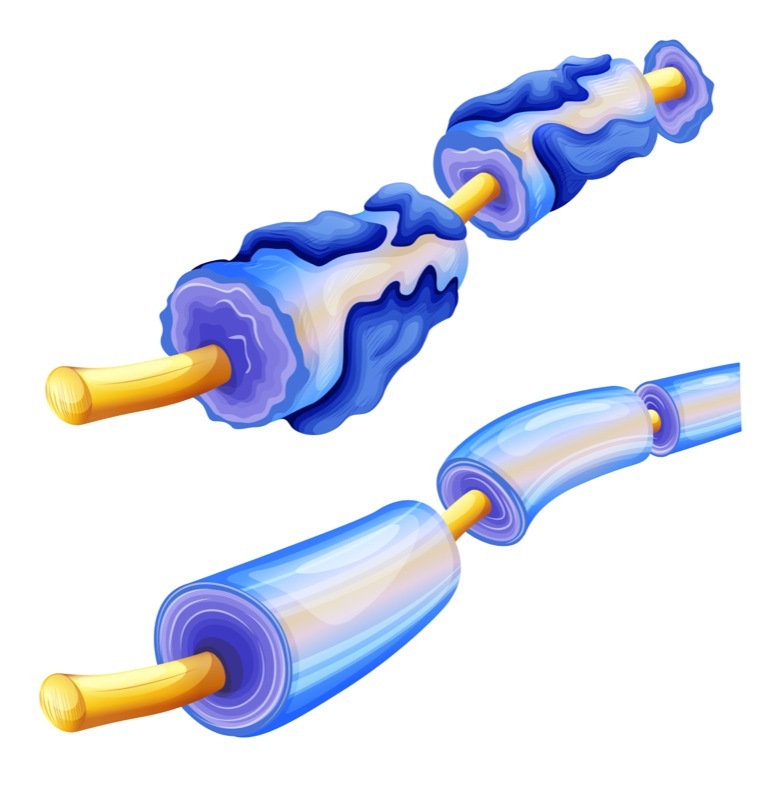
The hallmark of MS is the immune system’s destruction of myelin, the coating that surrounds nerve cell axons (the long threadlike part of a nerve cell) and, much like the insulation around electrical wires, protects the axons and allows the firing of signals between nerve cells or between nerve cells and effector cells, like those in the muscles.
Destruction of myelin impairs the communication between nerve cells and eventually leads to their death. As such, one of the strategies for MS therapies is to find ways to promote the regeneration of myelin (remyelination), thereby preventing the death of nerve cells.
While remyelination occurs spontaneously in MS lesions, it becomes increasingly incomplete and eventually fails.
Discuss the latest research in the MS News Today forums!
During the development of the brain, there is an active production of myelin (myelination) by cells called oligodendrocytes, where a growth factor (called neurotrophin brain-derived neurotrophic factor, or BDNF) is vital.
BDNF binds to a receptor sitting at the surface of oligodendrocytes, called TrkB, to promote myelin production.
Using a BDNF-like molecule that activates TrkB at the surface of oligodendrocytes is therefore a potential strategy to restore myelin production in myelin-depleted brains.
Researchers at the University of Melbourne in Australia took advantage of the known structure of BDNF to develop a synthetic small molecule (peptide) that mimics the particular lock and key features of the binding of BDNF to TrkB.
This interaction occurs via a specific sequence of aminoacids (protein’s building blocks) that lead to the formation of loop structures. TDP6 mimics the loop structures of BDNF.
But the TDP6 peptide has advantages over the natural BDNF — it is smaller and more stable and was designed to specifically target the TrkB receptor.
In a previous study, researchers confirmed that BDNF and TDP6 enhance oligodendrocyte production of myelin in vitro. Now, they tested the capacity of BDNF and TDP6 to promote remyelination in a preclinical mouse model of central nervous system demyelination.
Following a chemical treatment to induce loss of myelin, mice received BDNF or TDP6 administered into the brains’ right ventricle, which is filled with cerebrospinal fluid, for seven days using a pump. Compared to control mice (infused with an innocuous solution), those treated with BDNF or TDP6 showed greater signs of remyelination.
A sign of the greater stability of TDP6 is the fact that researchers were able to detect it after seven days.
TDP6 also increased the numbers of oligodendrocytes and the thickness of the new myelin sheaths after a demyelinating “insult” — new myelin is usually thinner. In fact, TDP6 was even more effective at enhancing myelin regeneration than BDNF.
Researchers conducted a final experiment and confirmed that TDP6’s effects are carried out via the TrkB receptor in oligodendrocytes. After the genetic depletion of TrkB, the TDP6-induced benefits were loss.
In the past, strategies to use BDNF as a treatment failed due to its size and ability to interact with multiple receptors. Also, BDNF is quite unstable.
Now, these findings show that TDP6 overcomes these limitations, and support its usefulness as a potential strategy to activate TrkB in oligodendrocytes to induce myelin regeneration.
“Our key focus is to develop new versions of TDP6 and to uncover the molecular interactions that occur within oligodendrocytes that mediate this enhanced remyelination effect,” study authors Jessica Fletcher, PhD, and Susan Northfield, PhD, wrote in a University of Melbourne news story.
“It’s the first step towards developing treatments that act like electricians — repairing the insulation that allows the electricity running our brain to work properly,” they concluded.


