Tecfidera Better at Preventing Relapses than Aubagio, Real-world Study Suggests
Written by |
Tecfidera (dimethyl fumarate) is more efficient at preventing relapses, and has a lower discontinuation rate than Aubagio (teriflunomide), according to a Danish study.
The study “Comparative effectiveness of teriflunomide and dimethyl fumarate: A nationwide cohort study” was published in the journal Neurology.
Aubagio (marketed by Sanofi Genzyme) and Tecfidera (marketed by Biogen) are two oral disease-modifying therapies used as first-line treatments for relapsing-remitting multiple sclerosis (RRMS).
Data from Phase 3 clinical trials supported the therapies’ approvals – Aubagio was assessed in the TEMSO (NCT00134563) and TOWER (NCT00751881) trials, and Tecfidera in the DEFINE (NCT00420212) and CONFIRM (NCT00451451) trials.
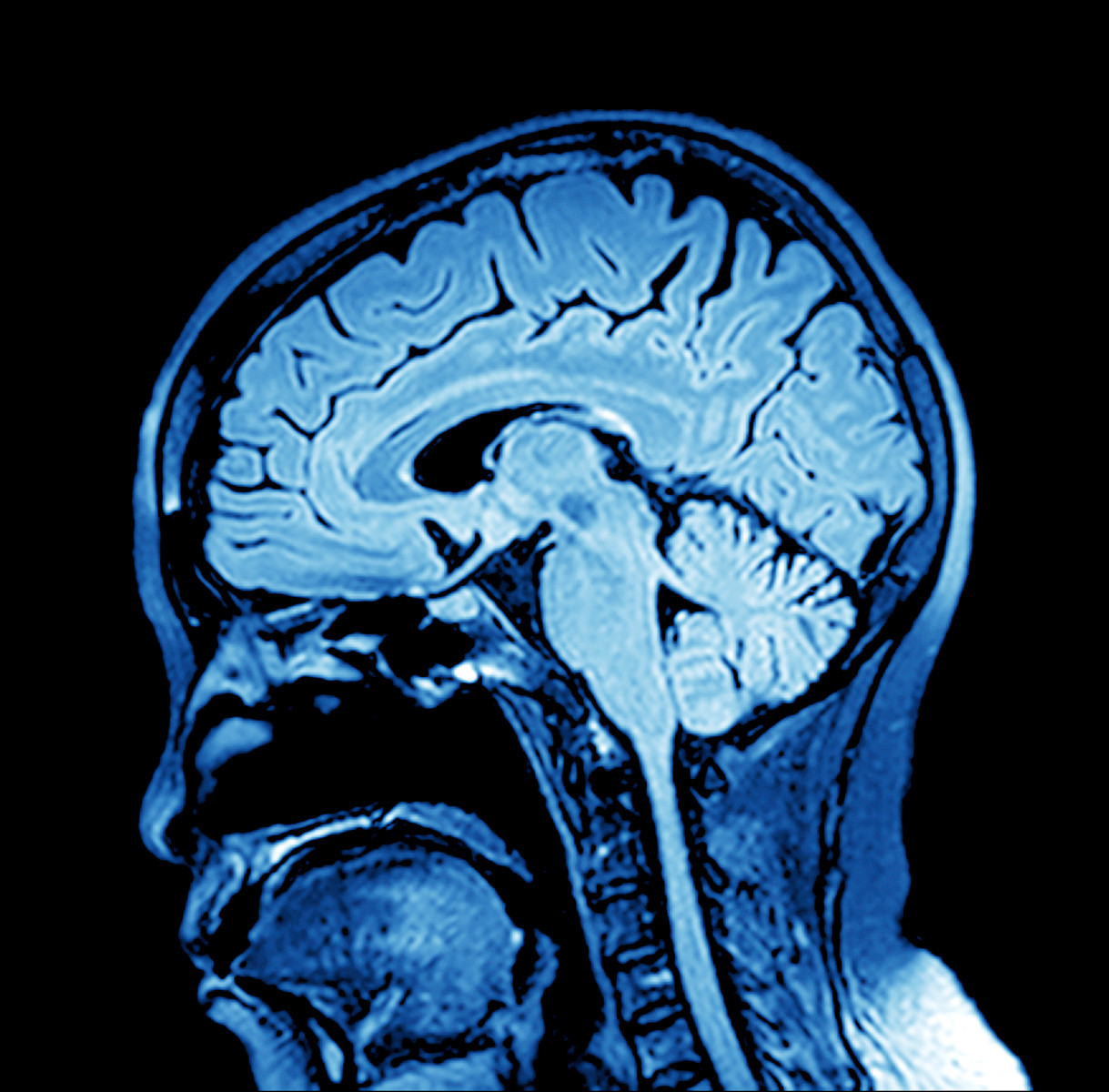
In summary, both therapies significantly reduced the annualized relapse rate (AAR) over two years, and the risk of 12-week confirmed disability worsening, compared to a placebo. Moreover, treatment decreased the number of new or enlarging active lesions, as shown by MRI.
However, head-to-head comparisons using real-world data assessing the effectiveness and safety of Aubagio and Tecfidera is limited. Pursuing this approach, however, “could provide important evidence for future treatment guidelines of patients with MS,” researchers wrote.
In order to make a direct comparison between the two therapies, researchers analyzed patients with RRMS registered in the Danish Multiple Sclerosis Registry who took Aubagio or Tecfidera from October 2013 to May 2018.
The analysis compared patient ARRs between both disease-modifying therapies, which was the study’s main objective. Secondary objectives included time to first relapse (the interval between treatment start and the first relapse), time to 6-month disability measured by the Expanded Disability Status Scale (EDSS) score (a measure of disability), reasons for discontinuation or switch, and adverse events (side effects).
The analysis included 2,236 patients — 1,469 were treated with Aubagio and 767 with Tecfidera — with a mean follow-up of two years. Patients treated with Tecfidera were, in general, younger and female, and more likely to have received treatment with other disease-modifying therapies.
During follow-up, a total of 433 and 175 relapses occurred in patients treated with Aubagio and Tecfidera, respectively. That corresponds to ARRs of 0.16 and 0.09, respectively.
Tecfidera was more effective at reducing ARRs, with patients showing an adjusted 42% lower relapse rate compared to Aubagio. In agreement with these results, the risk of having a first relapse also was lower in patients treated with Tecfidera.
Researchers saw no differences in disability score worsening between both treatments.
Treatment discontinuation due to disease worsening was higher in patients treated with Aubagio (22.1%) compared to Tecfidera (10.2%), reflecting the higher relapse activity seen in the Aubagio group.
Overall, researchers found a “lower ARR, higher relapse-free survival, and lower incidence of discontinuation due to disease breakthrough on treatment with DMF [Tecfidera] compared with TFL [Aubagio],” they wrote.
The team concluded that “for patients with RRMS, DMF [Tecfidera] is more effective in preventing relapses…compared with TFL [Aubagio].”


